Living With Cancer: Vicky’s Story
Vicky Bolton is a 58 year-old medical legal coordinator who lives in Albuquerque, New Mexico. A widower of 20 years, Vicky has three children and nine grandchildren. She is also a Stage 4 adenocarcinoma lung cancer survivor who receives treatment at New Mexico Cancer Center (NMCC) in Albuquerque. She was previously diagnosed with adult onset asthma 14 years ago, but her pain and breathing problems became progressively worse.
Three years after her asthma diagnosis, Vicky returned to her primary care provider about the pain in her lungs and was immediately referred to a pulmonologist for biopsy. The pulmonologist was unable to perform the biopsy because of concerns of fluid in the lungs and referred her to a vascular surgeon. The surgeon admitted her to the hospital to perform the biopsy and found that half of the lung was blocked from fluid and cancer, which had metastasized. The surgeon referred Vicky to NMCC and an oncologist met her in the surgery ward.
After starting their relationship 11 years ago, Vicky has been consistently receiving treatment at NMCC. In 2003 she started chemotherapy first with paclitaxel (Taxol) and then carboplatin, but was found to be allergic to both. Her oncologist switched her to gemcitabine (Gemzar), but complications with that chemotherapy agent culminated with a hospitalization in 2006 following kidney failure. Since 2006 Vicky has not been hospitalized, and only had to go to the emergency department or urgent care a few times for breathing problems. She has undergone additional chemotherapy, radiation therapy, and multiple rounds of injectable antibiotics, but all of these services were provided at NMCC’s facilities instead of in a hospital.
NMCC provides all of Vicky’s care at one location, from lab and x-ray testing to an internal medicine doctor for her recent stomach problems. The extended hours clinic has allowed her to get care outside of work hours, so that she can live with cancer rather than plan around it. In the past six months alone, NMCC prevented Vicky from being hospitalized on three occasions:
In December 2013 she became acutely ill. Although she was out of work for more than a week, she was able to receive all her treatment at NMCC and go home in the evenings and be with her family.
In February 2014 she was diagnosed with bilateral deep vein thrombosis, one of which was infected. On the same day NMCC infused her with daily antibiotics as an outpatient, allowing her to remain in the comfort of her home overnight.
In April 2014 she become ill on a Saturday and called NMCC’s extended hours clinic. On the same day, they performed lab work and radiology studies, and infused medications intravenously. NMCC continued to treat her in the evenings after work, allowing Vicky to attend her company’s annual meeting that week. During this time, Vicky missed no work days.
![]() Empowering the Patient During Cancer Treatment
Empowering the Patient During Cancer Treatment
Andrene Taylor, Cancer Survivor and Director, ZuriWorks
Part I: Introduction
According to the National Cancer Institute there are more than 13 million people living with cancer in the United States; it is the second leading cause of death in the U.S.1 It is expected that 41% of Americans will be diagnosed with cancer at some point during their lives. More than 1.6 million new cases of cancer will be diagnosed in 2014; a nearly 22% increase over the last decade.2
Cancer care is also expensive. In 2010 it accounted for $125 billion in health care spending and is expected to cost at least $158 billion by 2020, due to population increase.3 In 2011 Medicare alone spent nearly $35 billion in fee-for-service (FFS) payments for cancer care, representing almost 9% of all Medicare FFS payments overall.4
Broadly speaking, problems in complex clinical care fall into two categories: deficits in knowledge (for example, lack of any effective treatment for certain brain tumors) and deficits in execution (for example, failure to treat breast cancer with a standard-of-care protocol).5 Delivery reform seeks to find opportunity in the latter problem type. Considering cancer care through this lens, there are many opportunities to improve outcomes and potentially lower costs, including better coordination of care, eliminating duplication of services and reducing fragmentation of care.6,7,8 In addition, almost two-thirds of oncology revenue derives from drug sales9, and pricing for drugs (calculated by the average sale price plus 6% profit for providers) may incentivize the use of the most expensive drugs rather than equally effective, lower-cost alternatives.
Promising approaches are being developed to deliver high quality care, improve the patient experience, and reduce costs for this condition and other chronic diseases. Care redesign strategies such as adopting team-based models, offering extended practice hours, providing triage to keep patients out of the emergency room, and implementing care pathways help providers address avoidable costs and maximize the value of care. Many of these strategies are not currently reimbursed in the FFS, volume-based payment system.
Consequently, much policy attention is focusing on payment reform. On the heels of the Affordable Care Act (ACA), and numerous quality and payment focused initiatives in the private sector, health care organizations need to enhance the competitiveness and efficiency of their system in the marketplace. Alternative payment models (APMs) such as Accountable Care Organizations (ACOs), bundled payments, and patient-centered oncology medical homes (PCOMH) are just a few of the initiatives supported by public and private payers to align care redesign and payment reform and encourage continuous improvement. This paper provides a comprehensive overview of the complex care associated with oncology and the alternate payment models which help support optimal care and encourage continuous improvement.
To support effective implementation of these strategies in practices throughout the country—including the identification of barriers and challenges—this case study examines the redesign of the New Mexico Cancer Center (NMCC) as one example of how a group of clinicians can implement change. This case study will focus on the care redesign model and potential payment reform options to sustain improvements at NMCC. With the aim to support the education of a clinical audience regarding how care innovations can be aligned with alternative payment models, this case will answer the following questions:
- What challenges or problems encouraged the organization to redesign cancer care?
- How did NMCC redesign care to improve quality, enhance the patient experience, and reduce costs?
- How can an organization prove they are improving quality and contract with a payer to maintain sustainability?
- How can alternative payment models sustain a community oncology medical home?
Care and Cost Challenges
 The U.S. spent $125 billion on cancer care in 2010.10 Patients with cancer receiving chemotherapy averaged $111,000 per patient per year in total medical and pharmacy costs, with drugs accounting for about 25% of costs.11 Compared with other conditions, patients with cancer receiving chemotherapy incur six times the annual cost of patients with diabetes and 26 times the cost of patients without cancer.12 For patients themselves, the cost of care is prohibitive, with potentially tens of thousands of dollars in out of pocket expenses. A national survey found that 25% of patients consumed most or all of their savings in dealing with their cancer and its treatment.13 Another study found that patients with higher co-payments were 70% more likely to discontinue their treatment, and 42% more likely to skip doses.14 Combined with costs due to lost wages and unemployment, the costs of care can be prohibitive for some patients to seek and adhere to treatment.
The U.S. spent $125 billion on cancer care in 2010.10 Patients with cancer receiving chemotherapy averaged $111,000 per patient per year in total medical and pharmacy costs, with drugs accounting for about 25% of costs.11 Compared with other conditions, patients with cancer receiving chemotherapy incur six times the annual cost of patients with diabetes and 26 times the cost of patients without cancer.12 For patients themselves, the cost of care is prohibitive, with potentially tens of thousands of dollars in out of pocket expenses. A national survey found that 25% of patients consumed most or all of their savings in dealing with their cancer and its treatment.13 Another study found that patients with higher co-payments were 70% more likely to discontinue their treatment, and 42% more likely to skip doses.14 Combined with costs due to lost wages and unemployment, the costs of care can be prohibitive for some patients to seek and adhere to treatment.
A number of disparities exist across age, gender, type of cancer, race, socioeconomic status and geography. For example, African Americans are the more likely to be diagnosed with cancer in four of the five most common conditions. They also have a higher mortality rate: 27% higher among men and 11% higher among women.15,16 These variations in care and outcomes reflect opportunities where care can be standardized and improved.
A. Improved Health Outcomes that Contribute to Unavoidable Costs
There are many factors that make cancer care expensive that cannot be changed without compromising the quality of care received by cancer patients.
Aging Population: Cancer is most common among people aged 65 to 74 (25% of all new diagnoses are in this age range), and thus incidence and expenditures will increase as the elderly population grows.17 The age 65+ population is expected to boom from 40 million in 2009 to over 70 million in 2030, causing an estimated 27% increase in cancer care expenditures.18 As older patients tend to have more comorbidities and poorer health in general, they can also have more complex cases.
Increased Cancer Screening: Increased access to care and recent screening guidelines likely will contribute to significantly higher costs of diagnosis and treatments. While such strategies may contribute to reductions in cancer-specific mortality in some cases (for example, 1 in 1000 women and 1 in 1000 smokers may survive due to mammography and chest CT screening), increasing diagnosis may also lead to expensive testing and treatment in other cancers without benefit. For example, thyroid cancer has seen large increases in diagnosis with no changes in mortality rate.
Increased Survival Rates: Five year survival rates have continued to increase over the past 40 years and show an increase from 49% in 1975 to 68% in 2010.19 This is due to several factors including improved diagnostic and treatment methods (though may also include a component of lead-time bias). While these are clearly favorable outcomes, they contribute to cost increases as people live longer and have potential recurrences.
Advances in Technology: Innovative treatments that provide improved care are constantly being developed and advances in genomics and targeted chemotherapy options have led to numerous new treatment options. The research and development costs per new drugs can range anywhere from $15 million to $13.2 billion21 and treatment costs can also be very high. For example Novartis’ Afinitor, a drug used to treat advanced kidney cancer costs approximately $10,000 per month.22B. Suboptimal Care that Contributes to Avoidable Costs
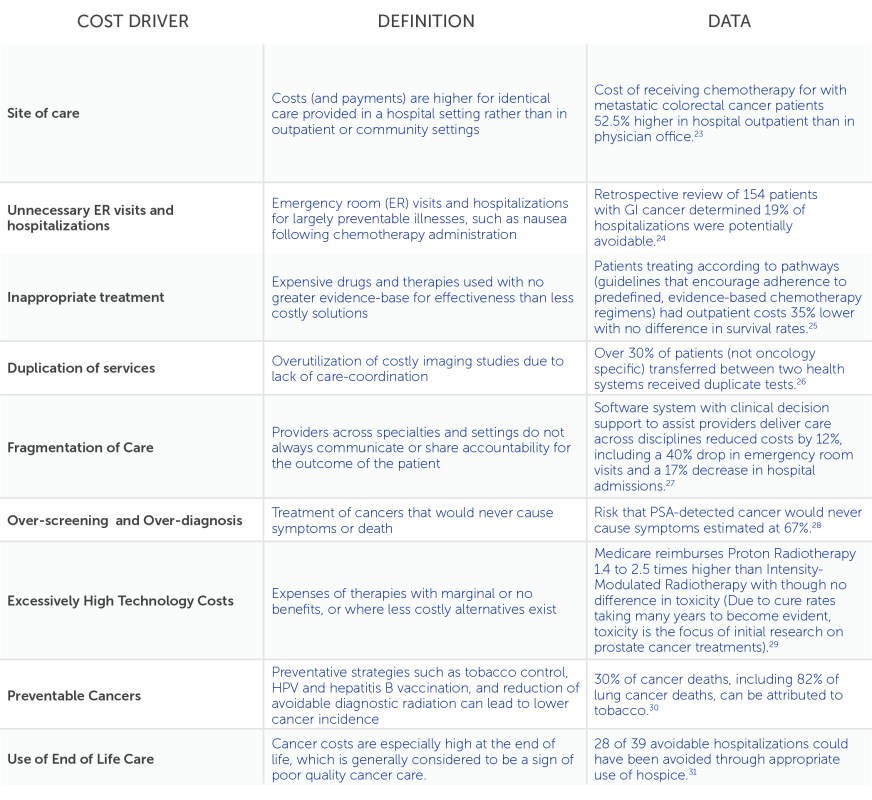
While some factors driving cancer costs are unavoidable or desirable, others are the result of poor care coordination and lack of evidence based care. These avoidable cost drivers are opportunities where payment reform can drive improved care delivery that can help reduce cancer care expenditures.
Overview of key contributors to suboptimal care and avoidable costs
 Cancer Drugs
Cancer Drugs
A specific issue in oncology costs merits special consideration. One of the greatest cost drivers in oncology is expensive cancer drugs. Federal policies regulating drug payment systems impact the financial solvency of practices and jeopardize the financial sustainability of care redesign. Under the “buy and bill” payment mechanism, providers purchase the drugs directly from pharmaceutical companies and are reimbursed for them later (includes average sales price for the drugs plus 6% for Medicare and variables for commercial payers). For many oncology practices, up to 65% of practice revenues result from this system.32 This payment mechanism incentivizes oncologists to prescribe more costly drugs to increase net revenues even when more cost-effective options are available. The undesirable added costs associated with more expensive cancer drugs are a controllable cost. Oncology practices like NMCC can implement care redesign to move toward prescribing more cost-effective cancer drugs, and these savings can be used to incentivize stakeholder buy-in.
Another mechanism that impacts drug pricing, and one that puts community-based, non-hospital practices at a cost disadvantage, is the 340b program. This requires drug manufacturers to provide 25 – 50% discounts on cancer drugs to community health centers (FQHCs), and allows the organizations to use the additional revenue made on more costly drugs to offset other costs. As a result organizations that cannot qualify for 340b status may be restrained in their relative ability to compete against other qualifying centers, which may limit investments in care redesign.
![]() The Future of Oncology: Drugs, Genetic Testing & Personalized Medicine
The Future of Oncology: Drugs, Genetic Testing & Personalized Medicine
Richard Schilsky, American Society of Clinical Oncology
Care Redesign Framework
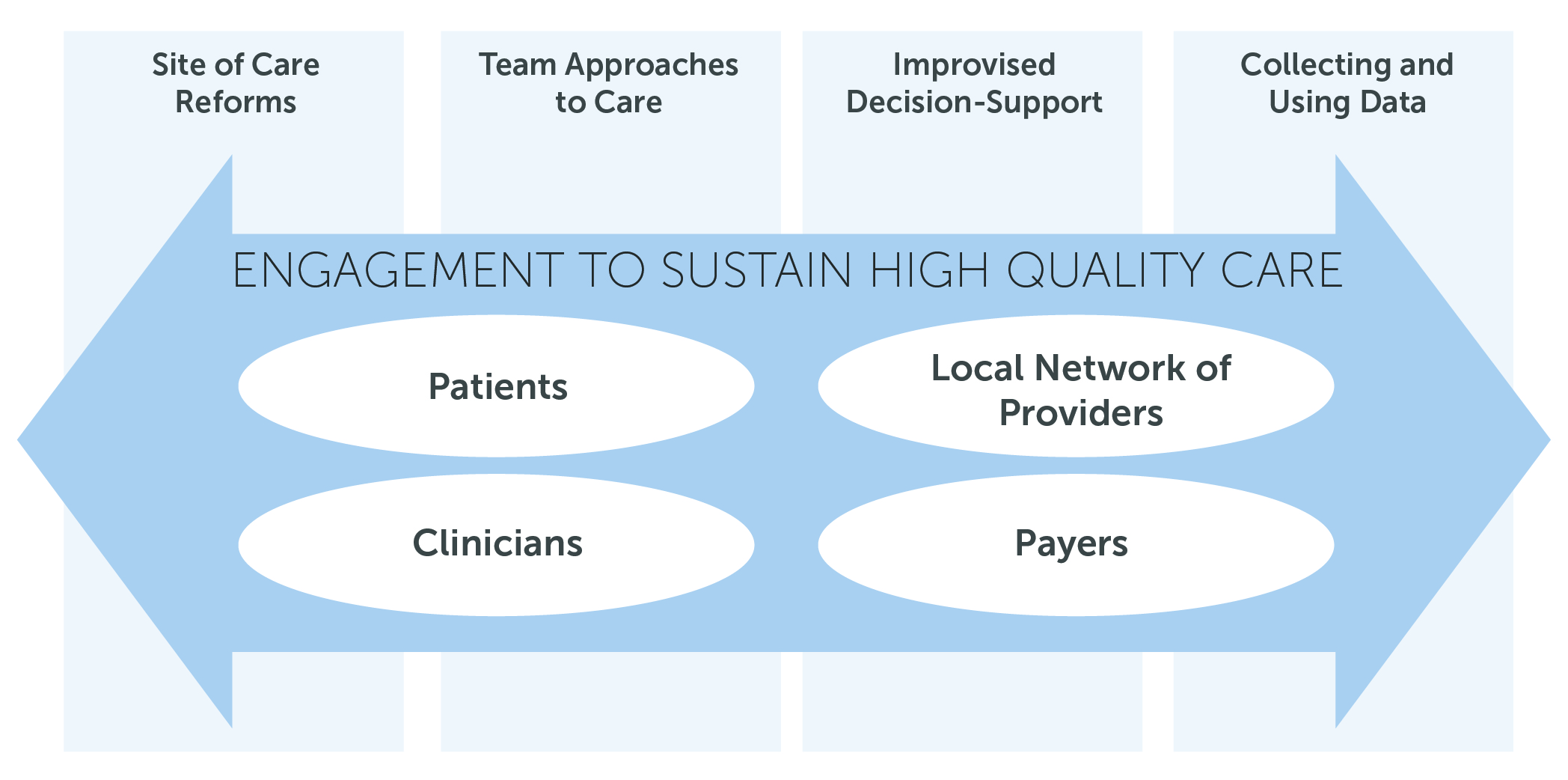
This case study uses a framework to consider these drivers of suboptimal care and the specific care redesign elements undertaken by NMCC to improve patient-centered care (Figure 3). All types of care redesign can be described in terms of where the care is delivered; who delivers the care; how are care decisions made; and which data are used to ensure effectiveness. To make any intended transformations ‘come alive’, extensive engagement is required across all stakeholders.33 Within a health care setting this will include patients, clinicians, the local network of providers, and those paying for care.
Data and Measurements
In general, payment is currently not tied to value in oncology care. To accomplish this transition to value-based payment, however, good measures of value must exist. Many organizations are developing performance measures. For example, the American Society of Clinical Oncology (ASCO), the Community Oncology Association (COA) and the National Quality Forum (NQF) each have specific oncology performance measures that practices can use to quantify the quality of care they deliver and determine areas for improvement. ASCO has also created the Quality Oncology Practice Initiative (QOPI) a performance benchmarking program with over 700 practices enrolled34 (35% of the estimated 2,000 oncology practices35). QOPI is also an approved registry for reporting the Physician Quality Reporting System’s (PQRS) oncology quality measures.
In addition to measures that are already developed, there are several areas in which work is underway to develop appropriate measures including: measurement of team approach to care; end-of-life and palliative care; patient-reported outcomes (quality of life, pain); and patient experience in care (refer to page 10, figure 4 in the case study PDF for a description of performance measure types).
Part II: Care Redesign and the Creation of the Community Oncology Medical Home
Dr. Barbara McAneny founded NMCC in 1987 and in her years working as a medical oncologist, she has been particularly frustrated by the adverse impact that fragmented care has on her patients. Often patients are directed to up to three different locations to receive care from their oncologist, lab, and chemotherapy provider. Cancer patients may also have to wait for hours in the ER before potentially being admitted.
This is particularly concerning for patients actively in treatment, since they experience frequent fatigue and are more susceptible to infection. Exposure to germs and infections can often have catastrophic outcomes. That this fragmentation has also led to many of the avoidable costs to the system outlined in the section above has added to her frustration. Dr. McAneny became dedicated to making major changes to the way that oncology care was delivered in New Mexico and in response created a free-standing, integrated cancer treatment that serves patients in a soothing and frictionless way.
![]() Aligning Clinical Redesign and Payment: The New Mexico Experience
Aligning Clinical Redesign and Payment: The New Mexico Experience
Barbara McAneny, New Mexico Cancer Center
Over the past fifteen years, NMCC has undergone extensive redesign to alleviate care fragmentation issues. This includes clinical improvement to change how care is delivered, infrastructure projects to change where care is delivered, and information and technology implementations to ensure effective measurement of change. Most of this redesign did not have direct financial support. The funding for these changes came from reinvestment of NMCC profits in the early 2000s. NMCC may have also benefited from the attraction of more patient volume due to their reputation for providing innovative cancer care. However, as payment rates have tightened and margins and profits have fallen over the past 10 years, this level of reinvestment is no longer sustainable for the practice under current payment models. While the changes made by NMCC had some impact on reducing fragmentation for patients, Dr. McAneny felt that more could and should be done to improve the patient experience, and to reduce the costs of cancer care. NMCC has, therefore, also attempted to work in a more integrated fashion with the wider New Mexico medical community.
Practice Environment and Local Health Care Market
NMCC competes in a complex environment in Albuquerque, NM. While New Mexico has a population of 2 million, almost half of the population lives in Albuquerque. Of the 50 hospitals across the state, most are small and rural, providing their local population with basic medical services. Specialist services, including cancer care are provided by three major health systems based in Albuquerque, including LoveLace Health Facility, Presbyterian Health Care and University of New Mexico Hospitals.
Until recently there were three main health plans serving Albuquerque: Presbyterian, Lovelace, and BlueCross BlueShield New Mexico (BCBS). Each of these plans had commercial managed care plans and government-sponsored (Medicaid and Medicare) managed care plans. In the fall of 2013 LoveLace lost its Medicaid contract to Molina Health and in the spring of 2014, sold its Medicare Advantage and commercial beneficiaries to BCBS, meaning Presbyterian and BCBS controlled over 60% of the Albuquerque market.36,37Working in Collaboration with Others
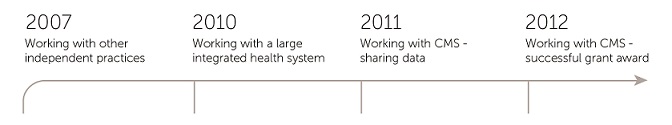
Over the years, NMCC has considered several strategies to work with providers and payers to change the way oncology care is delivered in New Mexico.
 A. Independent Medical Practices: Early ACO Efforts
A. Independent Medical Practices: Early ACO Efforts
In 2007, the NMCC leadership attempted to set up Independent Doctors of New Mexico (IDNM); a multi-disciplinary contracting vehicle with other independent physician groups, operating within a framework that included elements of both clinical and financial integration. The goals of the IDNM include: (1) Develop infrastructure to allow independent practices to compete with large vertically integrated systems; (2) Attain a degree of clinical integration to both make health care more efficient and affordable, and to meet governmental and quasi-governmental requirements; (3) Offer group purchasing opportunities not available to independent medical practices; (4) Establish a contracting vehicle to ensure an informed approach to managed care contract negotiations; (5) Support physician investors in their efforts to provide quality healthcare while staying economically viable; and (6) Encourage new insurers and new health care facilities to enter the market.
IDNM developed a web based portal for medical claim processing which included electronic claim submission to the clearing house, handling of remittance files from payers and generation of claim payment advice. While over 100 physicians signed up to the framework by 2008, IDNM was ultimately unsuccessful as a project as they were unable to find a payer to contract with them.
B. A Large Integrated Health System
NMCC previously reported a cooperative relationship with Presbyterian, and in 2010 decided to explore whether they could better address the issues of fragmentation of care by forming a closer working relationship. NMCC analyzed their data for Presbyterian health plan patients and compared this to industry standard data. Through looking at patients’ length of stay in hospital, NMCC estimated that they had saved the health plan approximately $18 million in the previous year. The response from Presbyterian was an overture to purchase NMCC for their provider arm.
NMCC’s leadership decided to not explore this arrangement as they felt that staying an independent, community- based center was better for their patients. The main driver in this decision was the belief that small community practices can make rapid changes to meet patient needs without the extensive layers of bureaucracy that can slow both the pace and scope of change. NMCC are also passionate proponents of the importance of independent practice as a key part of the delivery of health care; the leadership had concerns about both the impact that a reduction in provider organizations would have on patient choice, and the potential conflicts which exist in a fully integrated health system between payer (aiming to keep costs manageable) and provider (aiming to deliver the best possible care). The analytical analysis undertaken as part of this process served to emphasis the impact that ER visits and hospitalizations had on NMCC’s patients and the high cost impact for the whole system.
C. CMS Innovation Grant
The Center for Medicare and Medicaid Innovation (CMMI) was established in 2010 by the Affordable Care Act as a new branch of CMS. The goal of CMMI’s initial $10 billion, 10-year budget is to develop and test new models for delivering and paying for health care. Since its formation, CMMI continues to develop ACOs, coordinate health care for dual-eligibles (low-income Medicare beneficiaries that also qualify for Medicaid), provide enhanced primary care services, and test bundled payments.38 One CMMI initiative, the Health Care Innovation Awards (HCIA), provides funding to health care organizations that are already improving health care and lowering costs for Medicare and Medicaid patients.
In 2011, Dr. McAneny was involved in discussions with CMMI. The discussion was centered on the CMS pilot projects which were struggling to show cost savings. Dr. McAneny shared NMCC’s cost savings analysis developed for the Presbyterian negotiations and was encouraged to apply for an HCIA grant to develop a ‘proof of concept’ for the community oncology model.
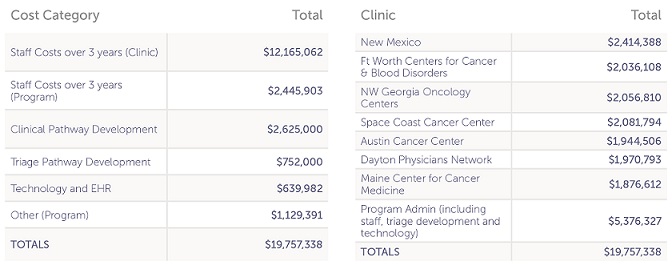
Dr. McAneny applied for the HCIA award along with six community oncology practices and, in order to distribute the grant and provide administrative oversight, she created a company called Innovative Oncology Business Solutions (IOBS). In 2012, the first round of awards gave a total of $1 billion to 107 health care organizations across the country, to explore how better care could be delivered in the most cost effective way. IOBS was awarded $19,757,338 to deliver the COME HOME program over three years.39
The grant focused on showing how community oncology practices could manage cancer symptoms and complications, and save money by reducing use of emergency rooms and preventing inpatient admissions. The grant program runs for three years from July 2012 and has an explicit aim to reduce ER visits by 52% and hospitalization by 21%.40 Specifically, the grant described how to reduce costs through symptom management; increased access to care; use of pathways; compliance tracking and better data management; and better management for additional cost efficiencies.
Overview of the COME HOME Model
 The program builds on, and acts as an extension to, the foundation of successful changes made by NMCC to develop a comprehensive model of community oncology care demonstrating improved outcomes, enhanced patient care and saved costs. The program is working with six other clinics across the country to generate a proof of concept for the model, relevant to different markets with an aim that the outcomes from the program can be used to generate ideas for long-term sustainable practice.
The program builds on, and acts as an extension to, the foundation of successful changes made by NMCC to develop a comprehensive model of community oncology care demonstrating improved outcomes, enhanced patient care and saved costs. The program is working with six other clinics across the country to generate a proof of concept for the model, relevant to different markets with an aim that the outcomes from the program can be used to generate ideas for long-term sustainable practice.
Target Population
The target population for the program is newly diagnosed or relapsed Medicare, Medicaid and commercial insurance patients seeking oncology care at one of seven participating clinics. The program aimed to enroll approximately a total of 9,558 patients during the three year project and as of March 31st 2014, has recruited 107% of target (total of 10,213 unique patients). Of these, 26% are NMCC patients.
![]()
Sustaining Patient-Centered Care through the COME HOME Model
Laura Stevens, Innovative Oncology Business Solutions
Projected Savings
The reduction in ER visits and hospitalizations are projected to produce overall Medicare cost savings of $4,178 per patient per year (PPPY), a saving of approximately 6.28%. Over three years, the project is expected to save Medicare $33.5 million and result in a net savings of $13.76 million (See Figure 9). NMCC estimated these savings based on a Medicare enrollment of 8,022 patients over the three years and used Medical Expenditure Panel Survey (MEPS) data to calculate the baseline costs per patient. The majority of the savings per patient will come from reduced hospital admissions but also from reduced ED visits and pharmacy costs. The increase in physician costs reflects the additional visits for acute symptom management that are an essential part of the COME HOME model.42Program Expenditures
The COME HOME Program funds both ongoing staffing costs and infrastructure development. Each of the participating clinics has 10.5 full-time equivalents (FTE) staff, in addition to the staff who work across the program itself. A key constraint of the grant money is that it cannot be used for any service which is billed with an Evaluation and Management (E&M) code through FFS, to guarantee that CMS is not paying twice at any point. The allocation of the 10.5 FTEs varies between the different clinics. At NMCC this funds 4.8 nurses, 0.4 data analyst, 1.75 patient care coordinators, 1.75 telephone triage operators, 0.75 front desk manager and 0.75 clinic manager.
Overview of project costs by category
Care Redesign Strategy
In this section, we consider NMCC’s redesign strategies using the delivery innovation framework that focus on four key success factors: site of care reforms, team-based care, improved decision support, and collecting and using data; all of which reinforce efforts to engage and educate stakeholders to ensure sustainability of high-quality care.
A. Site of Care Reforms
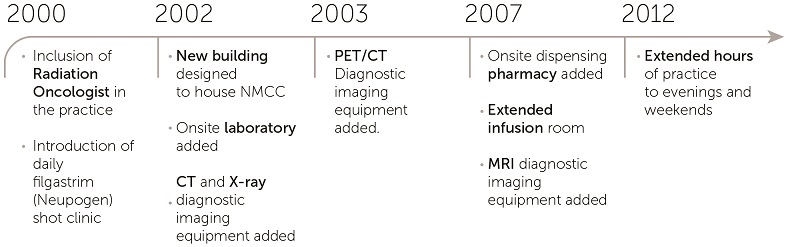 Design a patient-centered facility. NMCC bought land to build their center in 2001 and the patient perspective had an impact in all areas of building design and décor. The center itself is a single-story building with a parking lot right outside so that patients do not need to walk a long way to and from their treatments. The internal layout of the building has also been designed to feel more like home, and less like an austere clinical institution. Rather than one large and overwhelming office, the doctors’ offices are arranged in three ‘pods’; and there is a main desk with medical assistants assigned to support patients and clinicians. After the building had been designed, further work was required to include all of the envisioned services. In 2002, they added an onsite laboratory and over the next several years purchased their own imaging equipment including CT, x-ray, PET and MRI equipment. In 2007, NMCC added their own dispensing pharmacy and expanded their infusion room to include a separate area for those who may need to lie down or require special medical attention.
Design a patient-centered facility. NMCC bought land to build their center in 2001 and the patient perspective had an impact in all areas of building design and décor. The center itself is a single-story building with a parking lot right outside so that patients do not need to walk a long way to and from their treatments. The internal layout of the building has also been designed to feel more like home, and less like an austere clinical institution. Rather than one large and overwhelming office, the doctors’ offices are arranged in three ‘pods’; and there is a main desk with medical assistants assigned to support patients and clinicians. After the building had been designed, further work was required to include all of the envisioned services. In 2002, they added an onsite laboratory and over the next several years purchased their own imaging equipment including CT, x-ray, PET and MRI equipment. In 2007, NMCC added their own dispensing pharmacy and expanded their infusion room to include a separate area for those who may need to lie down or require special medical attention.
Provide all services in one community location. Geographic clustering of care can lead to better patient satisfaction and less duplication of services; it allows for better medication management, lab testing, and follow-up care. By providing patients with a “one stop shop” for all their services, patients are no longer overwhelmed by visiting multiple sites and hard to navigate buildings. Further, by providing this all in a community setting, NMCC ensures that the rates paid for services are lower than they would be in a hospital inpatient or outpatient department. For example, the per beneficiary cost of receiving chemotherapy in a hospital is 25 to 47% higher than in a physician office. While these improvements were successful, NMCC wanted to focus further on reducing unnecessary ER visits and hospitalizations.44
Provide easy access to routine services. Chemotherapy harms the body’s infection-fighting ability, which is treated by filgastrim (Neupogen) injections to enhance the number of immune cells to prevent fever and infection. Prior to the implementation of NMCC’s weekend shot clinic, patients had to visit the ER or inpatient facility; pay higher costs for treatments and co-pays; and often waited for several hours in an infection-prone environment. With COME HOME funding, NMCC expanded shot clinic hours and services to include management of fever and other Neupogen side effects to mitigate unnecessary hospital or ER visits (anecdotal evidence suggests that it is).
Coordinate care with local hospital. When admitted or seen in a hospital, many cancer patients undergo unnecessary repeated radiography and other expensive testing and treatment. To avoid this, NMCC employed a hospitalist to care for all NMCC patients in one ward. This greater coordination of care avoided unnecessary repeat testing, ensured good handoffs and communication with primary oncology teams, and avoided cancer treatments interrupted by hospitalization.
Expand access through after hours care. The most significant site of care change was extending practice. Prior to the COME HOME project, NMCC closed at 5pm on weekdays and offered no weekend hours. The center is now open until 8pm on weekdays and 1pm – 4pm on weekends (including the shot clinic). In addition to the physicians and nurses operating at these times, physicians have access to tests and results required to treat. The on-site lab is also open to ensure that patients are treated effectively. NMCC also hired an urgent care physician to treat patients experiencing side-effects. At the end of quarter seven, NMCC has averaged 82 extended hours’ visits per month accounting for approximately 14% of all patient visits.
B. Team-Based Care
 Add care coordinators to care teams. Each physician is paired with a patient care coordinator (PCC), with whom they share a case-load. The PCC takes all routine non-clinical work from the doctor so that they can work at the top of their license. They also work with patients to book appointments, schedule required treatments, and arrange travel when necessary. This helps reduce delays in treatment and allows the patient to focus solely on their treatment and recovery.
Add care coordinators to care teams. Each physician is paired with a patient care coordinator (PCC), with whom they share a case-load. The PCC takes all routine non-clinical work from the doctor so that they can work at the top of their license. They also work with patients to book appointments, schedule required treatments, and arrange travel when necessary. This helps reduce delays in treatment and allows the patient to focus solely on their treatment and recovery.
Clinically trained administrative staff. All administrative staff operate as medical assistants, ensuring that they are able to appropriately support patients through the complex check- in process when they visit the clinic. This also means that they operate as part of the clinical team, reducing the common divide between clinical and non-clinical professionals.
Financial counseling added to patient care regimen. Every new oncology patient meets with an on-staff financial counselor; NMCC feels that it is essential to provide these services early on to prevent patients from disrupting their treatment due to the high cost. This initial meeting reviews the details of the patient’s insurance plan to determine what will be covered and what the patient must pay out of pocket. Between doctor visits, lab tests, treatments, procedures, imaging tests, drugs and other costs, there are many different aspects of an insurance policy to consider which can be very confusing for patients. Beyond treatment costs, many patients may experience other financial consequences or limitations as a result of not being able to work, paying for additional childcare or transportation to and from doctor visits. The financial counselor provides patients with information about treatment costs and connects them with local resources that can provide financial assistance.
C. Improved Decision Support
NMCC has worked to improve their decision support for both physicians and nursing staff. Physician support has been focused on diagnostic and therapeutic pathways, a set of guidelines that steer physicians toward the most effective treatment, and toward the most cost-effective one when two treatments are equally effective. Nursing support has focused on triage pathways. In a nationwide study from 2012, over half of all payers have implemented oncology pathways programs or had plans to do so over the next two years.45Diagnostic and Therapeutic Pathways. In 2008, NMCC analyzed treatment regimens and recognized that there was more variation in the diagnostic and therapeutic pathways used by physicians than was ideal. They completed a collaborative exercise across their physician group to explain the variance, and developed best-practices to consolidate pathways covering the majority of oncology treatment plans. For example, without standardization and consensus building, two physicians treating two female patients with early stage breast cancer and identical clinical profiles, may still prescribe treatments of varying cost or outcome.
As oncology pathways become more common, several vendors have developed pathways as products. Many of these companies market their pathways directly to payer organizations as a way to help them get their cancer drug costs under control. Some also sell directly to providers who are interested in implementing pathways. NMCC estimated the cost of purchasing pathways from one of these vendors to be approximately $10,000 per physician per year.
While NMCC considered purchasing pre-existing pathways, they eventually decided to develop their own in order to retain flexibility and to support physician engagement. Through COME HOME, each practice is paid $125,000 to collaborate on pathway development. They have partnered with KEW Group and created the KEW Oncology Network. Meetings are held on a quarterly basis with representatives from all seven practices. During these meetings, representatives determine and choose which treatment is the most clinically effective with the lowest toxicity, and where other factors are equal, and which therapies are most cost-effective. This program has created pathways for the seven tumor types, which together account for 75% of NMCC’s oncology patients.46
NMCC physicians are currently at 80% adherence to their pathways and have started to look at other measures for diagnostic and therapeutic excellence. They introduced a new measure in March 2014 to identify the number of patients who are “staged” within one month of diagnosis. Currently they are meeting this target for 23.8% of patients, and are now working toward revised target of 50%, and anticipate achieving 100% over time.47 (This actual rate of staging compliance may be underestimated due to a delay in migrating this statistic to a searchable field in their electronic medical record).
Triage Pathways. The most significant decision support reform was the introduction of triage pathways for telephone support when patients would call with acute symptoms or questions. Previously, only experienced oncology registers nurses (RNs) and licensed practical nurses (LPNs) provided patient assistance via telephone and calls were limited to the hours of 8am and 5pm, and there were no formal written processes. This led to lengthy calls with patients, variation in the information patients were given, and possible preventable ER visits and hospitalizations. The new process uses a web-based interface that pulls data twice a day from NMCC’s electronic health record (EHR) system. Telephone operators receive calls, and nurses guide patients through a pathway; a course of pre-defined questions based on the patient’s inquiry. All triage staff are funded through the grant.
Implement real-time decision support. While the initial goal of the triage process was to address patient needs before sought treatment in the ER, it subsequently evolved into an automated decision support system for active symptom management. Triage enables automated, real-time decision-making support for the nursing staff. The pathways were both developed by a team of physicians and nurses, and are updated continuously. To ensure pathway compliance, they are monitored closely, and any falloff triggers the team to consider updating the pathways.
For example, one analysis demonstrated that patients with pain and nausea were refusing to attend same-day appointments and then later visiting the ER. The pathways were subsequently modified to include a follow-up call if the patient refused to make a same day appointment. When nurses called the patient back later in the day to check on their pain and nausea, nurses would again highly encourage patients with persistent symptoms to come to the clinic that day. As a result, patients began visiting the clinic rather than the ER. By the end of the seventh quarter, NMCC was averaging 950 triage phone calls, and using 300 pathways per month. Triage pathway compliance was running at 74.92% against a target of 80%.
D. Collecting and Using Data
NMCC has focused on actionable data. Before any data is collected, a schema is developed outlining the intended use and the decisions it will reinforce. That is, NMCC uses the data collected to produce measures that enable clinical actions to improve care. Quality measures are not considered static and once achieved, are amended with more rigorous targets.
NMCC would like to use claims data from CMS and other payers to help identify opportunities for improvements in care, but they have not managed to solve some of the key data sharing issues involved, including privacy concerns and the timely access to information.
Collecting patient surveys. NMCC uses a patient satisfaction survey developed by Community Oncology Alliance (COA), based on the Consumer Assessment of Healthcare Providers and Systems (CAHPS) methodology.48 The COA survey includes questions that could be turned into quality measures for actionable data and focuses on (1) whether patients received their care right away; (2) whether patients received all the information they wanted about their health to share in decision making; and (3) whether patients felt they were treated with respect.
Effectively adopt and use health information technology. NMCC’s EHR was originally purchased as part of NMCC’s profit reinvestment in the early 2000s (the initial cost was approximately $450,000 and the practice spends $500,000 annually for licenses and maintenance). The diagnostic, therapeutic, and triage pathways are integrated into the EHR, which provides real-time reporting with twice-daily data sync. Recent improvements to the system include ability to input DNR discussions (a key quality metric), co-morbidities, and family history. NMCC also assessed EHR meaningful use requirements when designing specifications. In future enhancements, NMCC intends to develop predictive analytics to target specific interventions.
5. Engaging and Educating Stakeholders to Sustain High-Quality Care
None of the care redesign changes highlighted above would be possible without effective engagement and education of patients, clinicians, and the local network of providers.
A. Patients
As described in the section above, NMCC uses patient satisfaction surveys as a key mechanism for engaging with patients. Their median patient satisfaction score using the COA CAHPS survey is 90.63%, compared to national scores of 62% to 82%. Changes made at NMCC as a result of survey responses include a major redesign of scheduling processes for the infusion room to reduced wait time from over an hour to about 6 minutes, and an increase in the number of patient education programs. In addition, integral to the COME HOME model is engaging with patients at every point of contact with NMCC. This includes encouraging patients to call into the triage line and to walk-in to the clinic if they need to. Many patients hold preconceived beliefs that by calling the doctor’s office, they are “bothering the doctor.”
Thus, in order for the COME HOME model to succeed, they have engaged patients and encourage them to take advantage of all the benefits that COME HOME offers. From the moment patients first enter NMCC they are greeted by staff wearing buttons advertising the COME HOME program. Every new patient has a half hour meeting with a nurse navigator during which they discuss the details of their condition and treatment, as well as the benefits of the COME HOME program. The purpose is to emphasize it is a unique program that creates a unique patient-centered experience. During this patient education meeting, each patient receives a notebook with detailed information about cancer that also explains the COME HOME program. They also receive a “Gold Card” listing phone numbers and hours of operation. Patient engagement is a center-wide effort that is based on a unified message from all physicians and staff. Every member of the NMCC team has been trained on delivering this message and is encouraged to remind patients of the importance of calling their doctor’s office first before visiting the hospital.
The New Mexico Cancer Center Foundation (NMCCF), a nonprofit organization, was created in 2003 to help patients with their non-medical financial needs while they undergo treatment. The foundation provides small grants to cover specific costs that will allow the patient to focus on completing their treatment, as well as educational programs on topics requested by patients. Last year the foundation’s budget was between $200,000 and $300,000. Patients can apply for a grant directly (maximum of $1,000 dollars per year) or they can be referred by clinic staff. No money is given directly to patients; instead the foundation will pay a specific bill (a mortgage payment, for example) or provide a gas card so that the patient can travel to the clinic. In the past year, NMCCF provided grants to nearly 200 patients. The Foundation has a variety of fundraising mechanisms to cover its budget. For example, NMCCF doubles as an art gallery with artwork on display year round that can be purchased at any time. Four times a year the foundation also holds art shows to display and sell its artwork to the public.
B. Clinicians
NMCC encourages transparency for productivity and quality data, which is shared among physicians. This includes numbers of overall patients, numbers of new patients, and scheduling. Despite the focus on quality of care, however, discretionary physicians’ bonuses are still calculated based on volume (measured by relative value units or “RVUs”). Non-partner staff were previously up to 50% of overall pay, though this percentage has since declined. Partners receive a profit-share based on their volume. At this point, the bonus and incentive system still relies entirely on productivity and clinical volume, rather than measures of quality, improved outcomes, or patient satisfaction. As part of the COME HOME program, the senior management team led the culture shift to patient-centeredness, with the extension of operating hours into the evenings and weekends. They worked with staffing groups across the disciplines and led best-practice improvement sessions in each team meeting to ensure that staff were appropriately ‘bought-in’ to the process. Physician involvement in developing diagnostic, therapeutic and triage pathways also ensured that they had ownership of major changes.
C. Local Network of Providers
NMCC maintains close ties with other providers in the community and also relies on an informal network developed through working relationships of NMCC staff. For example, their internist has been practicing in New Mexico for 40 years in a variety of settings and has maintained good relationships with physicians outside of NMCC. These relationships are essential to communicating with primary care offices about the services their patients are receiving at NMCC. Rather than patients going to their primary care physicians with specialized complications, they can receive treatment at NMCC where there is more oncology expertise. There would be great benefit to formalizing some of these relationships, particularly in mitigating risk if key staff left the practice. However, a broad lack of technological interoperability prevents NMCC and outside providers from sharing data about their mutual patients. There is also a lack of financial support available for coordinating care across many organizations. An additional area for improvement would be their connections with long-term care and hospice care organizations. NMCC does not have any direct or informal connections with these facilities which hinders their ability to fully coordinate patient care.
Part III: Payment Reform
 The key challenge for NMCC is to be able to show evidence that the model has reduced unnecessary ER visits and hospitalizations, and prove its financial viability. In this section we provide an overview of the payment models available to NMCC and discuss which approaches may be the most suitable for sustaining their practice moving forward. NMCC currently receives approximately $70,000 per month from the CMMI grant, and has not yet identified a clear strategy to sustain the delivery reforms in the COME HOME care model past the conclusion of the funding cycle (July 2015). A further challenge is that the grant does not actually cover all of the extra costs for the extended practice hours (CMS cannot be billed for the same activities twice, so CMMI grant funds cannot be used toward activities that are billed as Evaluation and Management (E&M) codes). The E&M code reimbursements do not include an additional payment for extended office hours yet NMCC are required to pay staff at a higher hourly rate for this work. This means that the grant only covers the full costs of triage nurses and operators, and some administrative staff and clinic managers.
The key challenge for NMCC is to be able to show evidence that the model has reduced unnecessary ER visits and hospitalizations, and prove its financial viability. In this section we provide an overview of the payment models available to NMCC and discuss which approaches may be the most suitable for sustaining their practice moving forward. NMCC currently receives approximately $70,000 per month from the CMMI grant, and has not yet identified a clear strategy to sustain the delivery reforms in the COME HOME care model past the conclusion of the funding cycle (July 2015). A further challenge is that the grant does not actually cover all of the extra costs for the extended practice hours (CMS cannot be billed for the same activities twice, so CMMI grant funds cannot be used toward activities that are billed as Evaluation and Management (E&M) codes). The E&M code reimbursements do not include an additional payment for extended office hours yet NMCC are required to pay staff at a higher hourly rate for this work. This means that the grant only covers the full costs of triage nurses and operators, and some administrative staff and clinic managers.
Current Cancer Payment Infrastructure
The majority of health care in the U.S. is reimbursed on a fee-for-service basis. This system rewards the volume of procedures rather than the value of care delivered, and services known to improve quality and reduce costs (care coordination, telemedicine, etc.) receive little to no reimbursement. In addition to these inherent issues, the current payment system does not reward quality improvement. Specifically, if a practice undergoes major quality initiatives that lower costs, typically, financial savings accrue to the payer, and not the individual practice. These misaligned incentives and the lack of financial return signify that many practices simply cannot afford to achieve clinical transformation without additional funding streams. Without a sustainable funding source, it will also be increasingly difficult to expand and maintain their augmented services and offerings. Alternative payment models are essential to support continued improvement and transformation of care.
Working with Payers
Forging good relationships and building trust with commercial payers will help in identifying the different pressure points existing across the organization in making a funding decision (Figure 14). Considering and responding to the payment reform needs of government health policy makers, both state Medicaid officials and federal Medicare officials, is also important. For example, both Medicare and Medicaid programs are seeking to control costs by implementing medical homes, updating prospective payment models, rebalancing long-term support services, and reducing unnecessary ER and hospital admissions. Clinical leaders should be aware of government payment reform opportunities, including major federal grants and Medicaid waivers.
Decision-making process within a commercial insurer

![]() The Commercial Payer Perspective: Oncology Payment Reform
The Commercial Payer Perspective: Oncology Payment Reform
Brian Kiss, Florida Blue
Alternative Payment Models
Alternative payment models (APMs) currently in development for oncology are in the early stages, but efforts are underway to move toward comprehensive episode or case-based payments, and alternative payment structures for services not reimbursed in a FFS setting. Broader or larger case-based payments may also provide stronger incentives to limit costs and implement delivery reforms that lead to cost reductions, but these payments may expose oncologists to greater financial risk. Consequently, implementing payment reforms that are viewed as feasible and desirable by both providers and payers is difficult. The four key alternative payment models in oncology are: clinical pathways, Accountable Care Organizations (ACOs), patient-centered oncology medical home (PCOMH), and bundled payments.

![]() The Public Payer Perspective: Oncology Payment Reform
The Public Payer Perspective: Oncology Payment Reform
Patrick Conway, Center for Medicare and Medicaid Innovation at CMS
A. Clinical Pathways
Clinical pathways are based on National Comprehensive Cancer Network (NCCN) guidelines, and are considered by many as the first step toward more comprehensive payment and delivery reform options in oncology. The other APMs described below include pathways adherence as part of their reform. The clinical pathways model itself uses an add-on per-patient payment to encourage adherence to predefined, evidence-based chemotherapy regimens. A provider adopts clinical pathways into their workflow and in doing so, agrees to use a preselected group of triage, diagnostic, and/or therapeutic treatments. For treatments that are equally effective, the recommended pathways will recommend treatment with the lowest cost. A provider has to meet a certain level of pathway compliance (usually 80%), but can go ‘off pathway’ to accommodate patient preferences and variation in disease development.
Preliminary findings from pilot studies of clinical pathways suggest the initiatives have slowed cost growth, reduced the frequency of unnecessarily aggressive treatments and do not worsen outcomes. One study of a cohort of lung cancer patients showed a reduction in drug costs of 37% over the course of the 12 month study. A majority of these savings were associated with adjuvant and first-line chemotherapy drugs with no cost saving found in second-line settings.49Reduction in overall cancer costs through implementation of clinical pathways

More conservative cost reduction estimates were announced by WellPoint, Inc, one of the nation’s largest health plans, which launched a clinical pathways payment program in July 2014.50 The program provides a $350 PMPM payment for each cancer patient treated through specific recommended pathways. WellPoint estimates the new program will reduce treatment costs between 3% and 4% annually. While pathways primarily result in a one-time savings after implementation, there is potential that their continued widespread use will disrupt the current pharmaceutical market and bring down the cost of oncology drugs overall. While pathways primarily consider efficacy and toxicity in choosing which drugs to recommend, cost is the final factor in determining which drug will be recommended. Drug companies may be compelled to consider the cost of their drugs in relation to those of similar efficacy and toxicity, which could lead to lower drug prices to be included in pathways.
Potential Opportunities and Barriers: NMCC developed pathways for seven tumor types as part of the COME HOME grant. They were not developed in conjunction with a commercial payer or with a commitment that CMS would provide PMPM fees for their use. Due to the earlier exercise undertaken in 2008 to consolidate their diagnostic and therapeutic pathways to reduce variation between their physicians, NMCC did not anticipate further overall cost savings from clinical pathways. Ultimately, NMCC views the new clinical pathways not as an APM in itself, but as an important quality initiative which will provide assurance to payers and encourage the use of APMs.
B. Patient-Centered Oncology Medical Home
The PCOMH includes a fixed PMPM fee for clinicians that meet a specific set of capabilities and quality standards in their practices, using an adaptation of the primary care patient-centered medical home framework established by the National Committee for Quality Assurance (NCQA). This fee can be used to support services not reimbursed through FFS or for infrastructure investments.
Reduction in overall cancer costs through implementation of a PCOMH

The initiation of the payment model begins with a patient’s diagnosis – when the practice assumes primary responsibility for the coordination of all services related to the cancer, and coordination with other providers for any non-oncologic care –and extends through to the survivorship phase of care. The case payment in oncology is generally between $200 and $250 PMPM which is significantly higher than the $5-$20 PMPM received in primary care due to the additional complexity of the care delivered to cancer patients.51
Preliminary findings from care and cost savings from PCOMHs have been promising. The most well-known PCOMH is pioneered by Dr. John Sprandio and his colleagues at the Consultants in Medical Oncology and Hematology (CMOH), a small physician practice outside of Philadelphia. In 2010, CMOH was the first oncology practice to be recognized by the NCQA as a level III PCMH.52
Early results showed that ED visits at the practice fell by 68%, hospital admissions for chemotherapy patients fell by 51%, and length of stay fell by 21%.53 These reductions are driven through promotion of care standardization and cost effective symptom management.54 CMOH estimates that the aggregated savings to CMOH payers is approximately $1 million per physician per year through reductions in the cost of care for the clinically vulnerable- patients that are older, chronically ill, and with multiple comorbidities. Despite signals that quality of care has improved, Sprandio suggests that the model is economically unsustainable under the current FFS without payer support.55Potential Opportunities and Barriers: There are several attractive aspects of the PCOMH model. Clinically, it aligns the interests of providers and engages patients to manage symptoms. It mitigates the possibility of acute events (such as an ER visit), so may decrease costs. NMCC is well positioned to implement this model because they already have in place many of the necessary quality measures (see Figure 18 that compares the current NCQA standards with suggested oncology specific goals). For example, they have a sophisticated IT infrastructure, an integrated EMR, a patient- centered culture, compliance monitoring, care coordination and follow-up processes. Although NMCC does not currently have NCQA certification as a PCMH, they appear to meet the criteria for Level III certification.
The fundamental barrier to adopting the PCOMH model is its validity as a sustainable payment alternative. The PMPM payment must be enough to cover the costs of the services provided that are not reimbursed through traditional FFS. NMCC must receive the PMPM upfront to continue its investment in services, staff, and enhanced hours. Currently, these costs are covered through the CMMI grant, but if the PMPM does not provide equivalent funding, NMCC might need to rethink their strategy moving forward. Data limitations and delays from CMS make it hard to establish the required PMPM, or determine how much NMCC will save the overall system if ER visits and hospitalizations are reduced. Conversely, without clear evidence that the up-front payment will lead to quality improvements that succeed in reducing overall costs of care, payers have been reluctant to agree to the additional payments.
Further, even if the technical issues facing a particular payer for NMCC can be addressed, it is unclear if any payer acting alone has enough market share to sustain the payment model. The medical home is difficult for NMCC to implement for only one payer’s patients, for both technical and professional practice reasons. If only one payer implemented the payment reform, the PMPM for supporting the medical home would apply to only a fraction of NMCC patients, making it difficult for NMCC to sustain the costs of maintaining medical home services and capabilities for their entire practice. While CMOH did eventually gain the support of local payers to sustain their practice in southeastern Pennsylvania, NMCC does not currently have such broad payer support in place.57 They started early conversations with BCBS about this model, but the discussions are currently stalled due to unresolved data-sharing issues.
C. Oncology Accountable Care Organizations (ACOs)
The oncology ACO framework introduces a shared saving model based on overall patient costs and quality of care in addition to FFS reimbursement. It builds on this alternative payment approach over time with an aim to moving more reimbursement from FFS towards a partially capitated payment for a broader range of oncology services. A group of providers are held accountable for the overall quality, cost, and care of their patient population and share the savings recouped fromm better coordinated, higher quality care. Early oncology ACO experiences have included specialty focused ACOs as well as oncology practices that are part of a broader, population health ACO arrangement. The high cost of cancer care and specialized nature of cancer services can create challenges in incorporating major aspects of oncology care into a population ACO model.
Reduction in overall cancer costs in an ACO

Two early oncology ACO models were developed in Florida with the local BCBS health plan, Florida Blue. The first was a collaboration between Baptist Health South Florida – a large health system with eight hospitals, and Advanced Medical Specialties – a large cancer center with seven practices, and the second was with Moffitt Cancer Center – a cancer specialist hospital with over 9,000 inpatient admissions per year and over 320,000 outpatient visits. There are approximately 1,000 patients across both ACOs and the model stratifies risk by cancer type. The models consider the patient’s total cost of care, not just oncology care, and bonus payments (on top of FFS) are on a per-member-per-year basis, running for one year from first diagnosis.58
A key challenge to developing these models was defining measurements – particularly how to define and attribute cancer cases. The sharing of data between provider and payer was crucial and outside counsel was required to address these and other issues (e.g., data privacy protections). The solution reached was to consider full utilization except mental and behavioral health and utilization and spending benchmarks were developed by actuaries within Florida Blue. The results of these models indicate early clinical successes and are on target to meet its goals of reductions in hospital admissions and readmissions, better generic drug prescribing rates, greater adherence to pathways and evidence-based protocols, and better coordinated care.59 The financial successes are less clear and, because of variations in costs of care, are difficult to discern with high statistical confidence.
Potential Opportunities and Barriers: The ACO model is an unlikely choice for NMCC. The biggest integrated payer-provider system in Albuquerque, Presbyterian Healthcare Services, and NMCC’s largest commercial insurer, has its own, hospital-based oncology practice and was a participant in the CMS’s Pioneer ACO program until 2013. Presbyterian left the Pioneer ACO program after the first year, but has continued to pursue other accountable care models outside of Medicare. The organization has not been able to reach a mutually agreeable ACO contract with NMCC.
NMCC’s next biggest health plan is BCBS of New Mexico. While NMCC has begun discussions with BCBS about proof of concept for the COME HOME program, the ACO model has not been part of these discussions because NMCC is small in size and scope, and does not have clarity regarding how they could take accountability for overall patient costs. In addition, NMCC’s experience with Independent Doctors of New Mexico in 2008, which could be considered to be an early ACO-type organization, and their recent experiences with Presbyterian, have led to a cautious approach to the ACO model. They are considering providing some oncology services to a local primary-care led ACO for one patient population, but are not considering the development of their own ACO.
D. Bundled Payments
A bundled payment is a combined payment for a package of clinically related services in a case or episode of care, including multiple services from a particular provider or the services of multiple providers. The bundled payment may be a fixed price paid prospectively, or a benchmark that is used to adjust net payments to the providers retrospectively. It is designed to appropriately compensate clinicians for the comprehensive set of services required to meet patient’s needs for the episode of care, as opposed to billing for each service separately. Bundled payments enable clinicians to redirect resources to services that are not currently compensated, and enforce accountability for the overall cost of the episode.
Reduction in overall cancer costs through implementation of a bundled payment model

There are many proposals for bundled payments in oncology, including a pilot focusing on multi-practice episode- based payment for chemotherapy drug administration (United Healthcare60) pilots for a broader set of bundled services for specific cancer types (Fox Chase and Horizon BCBS61, and 21st Century Oncology and Humana62), and a pilot for bundling radical prostatectomy for early stage patients (Mobile Surgery International and Florida Blue). Most of these pilots involve limited or partial shifts of FFS payments into episode-based payments. While CMMI is exploring bundled payment options for acute and post-acute care through the Bundled Payments for Care Improvement (BPCI) Initiative, the payment options do not include or target comprehensive cancer care.63
Each of these pilots has taken a different approach to the specific services incorporated into the bundle. UnitedHealthcare recently released results of a 3-year, 5 site pilot program which enrolled 810 patients into one of the bundled, prospective cancer care payments related to specific cancer stages for breast, lung, and colon cancer. (A total of 19 bundles were designed to cover various stages.) The payer reimbursed practices for all cancer chemotherapeutics at cost (no mark-up), but provided a prospective payment that covered inpatient and other care. Though drug costs rose, the overall care costs decrease by 34 percent, for a savings of $33.36 million, or roughly $41,000 per patient.64Potential Opportunities and Barriers: NMCC has not been able to assess the extent to which it could take on accountability for the costs of a bundle of services because it does not have access to complete claims data needed. As noted above, payers have been unable or unwilling to share this information with them. Even with the data, NMCC is not certain that it has the actuarial capacity to analyze this data appropriately.
Additionally, early understanding of which patients and services do or do not fit into a bundle is challenging, especially for broader bundled payments, and would require near-to real-time monitoring across the network for providers included in the bundle. Such systems are not currently in place. Further, NMCC expressed concern that implementing a broad bundle is made even more complex by the fact that treatments are constantly developing and changing – treatments that are standard now may be quite different in a year’s time. While some organizations have begun work on creating comprehensive bundled payments for cancer, only more limited bundled payment pilots like those described above are currently in operation. NMCC believes that these limited payment reforms may not be sufficient to support the major care reforms it has envisioned to achieve better outcomes and substantial savings. However, implementing an oncology medical home with supporting payment could be a basis for developing the data and systems needed to support effective implementation of bundled payment.
Part IV: Recommendations & Lessons Learned
In this section, we present recommendations for feasible alternative payment options at NMCC, which may help other organizations evaluate payment reform options at their own institutions. In Appendix A, we include a practical tool that provides a sample cost-benefit model, and data collection and strategic planning questions to help organizations assess their capacity and business case for care redesign.
A. Recommendations for Sustaining Change at NMCC
The APMs described in Part III present unique opportunities and challenges in supporting a sustainable payment strategy at NMCC. The goal is for the payment model to recover the amount of initial investment and support the COME HOME program’s ongoing costs and services at full capacity. Because no payer has a substantial market share (divided between Medicare, Presbyterian, BlueCross BlueShield, and others), payers may be reluctant to subsidize a service which could potentially be underwritten by another payer. Of payment reform options, NMCC has been unable to contract as part of a comprehensive ACO due to local health care market conditions. Clinical pathways are geared primarily to guidelines and chemotherapy adherence, and are not designed to provide funding for after-hours care or triage programs that are intended to achieve offsetting savings through avoiding costly complications. NMCC’s remaining options include:
Option 1: PCOMH with Accountability
Using the data it gathers, NMCC intends to quantify the additional costs the COME HOME model requires, and the savings that it achieves. Using that estimate, NMCC could suggest a PMPM payment from a private insurer to cover the costs of providing higher quality care. To encourage participation, NMCC could also enter into a risk-sharing agreement, in which overall costs of inpatient care and ER visits would be compared against a target. The PMPM could be at-risk if the targets are not achieved after a certain period of time. Recently CMMI signaled an interest in developing this type of model and specific details should be forthcoming in the near future.
Option 2: PCOMH with Accountability to Support Transition Toward Bundled Payment
While an oncology bundled payment is NMCC’s long-term preferred model, an interim possibility might be to use the medical home approach with risk sharing (described above) as a first step toward a bundled payment system. Developing reasinable cost estimates would require merging claims data with clinical data (for example, ICD-9 codes fail to distinguish between subtypes of breast cancer that have radically different treatments). A limited bundled payment pilot might be performed initially for high volume cancers, such as breast and lung.
Option 3: Enhanced FFS through Public or Private Insurance
NMCC could seek to modify the existing model with enhanced fee-for-service payments to cover out of hours visits and telephone-based triage services. However, this simply adds to the fee-for-service arrangements, and payers may be reluctant to support due to concerns that it would primarily generate additional billing rather than better care coordination, care transformation, and reductions in overall costs.
Option 4: Direct Contracting with Major Employers
Finally, given the challenges of working with payers in its market, NMCC could consider directly contracting for oncology services (“carving out”) with major employers (see Figure 21 for a list of the largest local employers). There is a precedent, in which Intel has entered into an ACO-type arrangement with Presbyterian Hospital to provide medical services to employees through the group health insurance sponsored by the employer.66 This would require collection of quality data and aggressive marketing strategies highlighting any cost, quality, and patient outcomes data to encourage adoption and strong competition.
Option 5: Commercialize the COME HOME Model
Another option that NMCC has to supplement income is to commercialize the strategies and triage software developed by Dr. McAneny through the COME HOME. By turning these products into commodities and marketing their potential to help organizations achieve the triple aim, they can be sold to other providers, perhaps leading to a durable source of revenue. This strategy would require further partnership with vendors, and possible additional capital infusion from investment partners. The advantage is that this strategy does not depend on payer cooperation, but the disadvantage is that (as with enhanced fee-for-service arrangements) there is little meaningful progress towards value-based payments from NMCC payers.
B. Lessons Learned
The experience of innovative pioneers like NMCC can shed some light on potential barriers to conceptualizing and implementing sustainable clinical redesign. The lessons learned have been sorted into three main categories: relationships with payers and networks, payment model selection, and data collection and quality improvement.
Relationships with Payers and Network
NMCC’s experience illustrates that a prolonged commitment to demonstrating significant value from care redesign, particularly from lower utilization of inpatient and emergency department utilization, does not automatically create a financial pathway for sustainable delivery reform. Innovative providers that seek to reform care should consider a sustainability path from the start. This might include involving lead payer partners early on to help identify end-points of interest to payers and potential payment alternatives to FFS that could support these reforms. Providing support for health care delivery reforms requires new activities by payers towards sharing data in new ways to enable care improvements to be prioritized and implemented, and aligning their payments with value, rather than volume and intensity of services. However, fragmented health care markets face challenges of the “free rider” problem (that is, payers may be unwilling to shoulder delivery transformation costs that may benefit other payers’ clients, and wait for CMS or others to make the financial investment, pay for the program evaluation, and enact policy change), payer inertia, and long lag times between care redesign and subsequent data demonstrating results.
Large ACOs and other integrated payer-provider plans, including those large enough to form Medicare Advantage plans, are moving forward on negotiating payment and delivery reforms. This may be more difficult for innovative, smaller practices, even if they can provide higher-value clinical services. However, reliance on very large providers may have anti-competitive consequences, such as discouraging delivery innovation that leads to “demand destruction” of high-cost hospital-based services. For this reason, private and public payers should be particularly interested in developing models that enable smaller, specialized providers like oncology practices to undertake key delivery reforms. Such specialty-specific payment models should be a high priority for CMS and regional or national collaborations on payment reform involving multiple private payers.
Payment Model Selection
While substantial attention has been paid to primary care focused APMs, specialty-focused APMs are needed for practices like NMCC. Their development should be a high priority for public and private payers. Clinical transformation grants, such as those offered by CMMI, should include clear pathways for transitioning to APMs if initial quality improvement and cost savings targets are met. Otherwise, delivery system innovations are at high risk of failure despite evidence of improved value. Another approach to help assure sustainability is for grants to require evidence of early payer engagement with delivery transformation efforts, and early implementation of key steps like the use of standard measures that could be a basis for APMs. Organizations such as ASCO have offered policy solutions for payment reform which could apply to both public and private payers as well as incorporating elements of bundled/episodic payments.68 These or other models now being implemented could provide a good foundation for “best practices” for smaller practices and payers to use to implement delivery and payment reforms at a much lower cost. Current oncology payers do not, as a rule, economically encourage strong beneficiary engagement as activated members of the care team, other than by requiring co-payment for emergency room care. Ideally, benefit design might also allow shared savings for beneficiaries for active participation in care or for seeking “right care in the place at the right time.”
Data Collection and Quality Improvement Considerations
Timely sharing of actionable information from claims and other administrative data remains a major challenge, with complex and varied procedures for obtaining claims from payers, and challenges especially for smaller practices in interpreting the claims data. Some states, such as Maryland, Massachusetts, Vermont, and Colorado are proceeding with creating all-payer claims databases.69 Maryland, for example, offers rapid provider feedback on some key information for patient management from claims through their CRISP database.70 Others, such as Minnesota, are using “distributed” approaches in which multiple payers and systems produce measures in consistent ways. Payers could also provide such data to innovative practices directly, to build trust and provide a needed foundation for payment and delivery reform.
In addition to producing performance measures from claims data, more progress is necessary to provide timely and actionable data to enable practices to improve performance. As NMCC’s early efforts illustrate, practices can produce more clinically sophisticated performance measures using the same clinical support systems that enable improved patient care. Strategies for getting to consistent methods for sharing key data on cost and quality need to be expanded to encourage quality improvement and payment reform.
Conclusion
Unfortunately those at the leading edge of change in the last decade are not necessarily in the position to benefit most from payment reform – they’ve already done a lot and there is relatively little low-hanging fruit – payers don’t want to have pay for changes already made. In fact, diminishing returns to quality improvement activities may actually be less costly for providers at a low baseline level or performance than for ones at a high level to improve quality.71
This means that providers who have either not engaged in significant delivery reform or those whose prices are already far above market averages stand to benefit the most from shared-saving arrangements, which tend to penalize those who already work efficiently. It also means that providers with high quality and low baseline costs must work that much harder if incentives are based on quality improvement as opposed to absolute quality.
DOWNLOADS
Full Case Study
Appendix A: A Model for Applying Reform to Your Own Organization
References & Endnotes