The addition of Medicare in 1965 completed a suite of federal programs designed to protect the wealth and health of people reaching older ages in the United States, starting with the Committee on Economic Security of 1934—known today as Social Security. While few would deny Medicare’s important role in improving older and disabled Americans’ financial security and health, many worry about sustaining and strengthening Medicare to finance high-quality, affordable health care for coming generations.
In 1965, average life expectancy for a 65-year-old man and woman was another 13 years and 16 years, respectively. Now, life expectancy for 65-year-olds is 18 years for men and 20 years for women—effectively a four- to five-year increase.
In 2011, the first of 75-million-plus baby boomers became eligible for Medicare. And by 2029, when all of the baby boomers will be 65 or older, the U.S. Census Bureau predicts 20 percent of the U.S. population will be older than 65. Just by virtue of the sheer size of the aging population, Medicare spending growth will accelerate sharply in the coming years.
Estimated Medicare Spending, 2010-2030
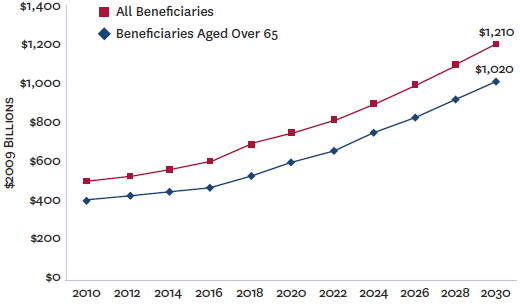
Sources: Future Elderly Model (FEM), University of Southern California Leonard D. Schaeffer Center for Health Policy & Economics, U.S. Census Bureau projections, Medicare Current Beneficiary Survey and Centers for Medicare & Medicaid Services.
The Center for Health Policy at Brookings and the USC Leonard D. Schaeffer Center for Health Policy and Economics’ half-day forum on the future of Medicare, looked ahead to the year 2030–a year when the youngest baby boomers will be Medicare-eligible– to explore the changing demographics, health care needs, medical technology costs, and financial resources that will be available to beneficiaries. The working papers below address five critical components of Medicare reform, including: modernizing Medicare’s infrastructure, benefit design, marketplace competition, and payment mechanisms.
DISCUSSION PAPERS
- Health and Health Care of Beneficiaries in 2030, Étienne Gaudette, Bryan Tysinger, Alwyn Cassil and Dana Goldman: This chartbook, prepared by the USC Schaeffer Center, aims to help policymakers understand how Medicare spending and beneficiary demographics will likely change over the next 15 years to help strengthen and sustain the program.
- Trends in the Well-Being of Aged and their Prospects through 2030, Gary Burtless: This paper offers a survey of trends in old-age poverty, income, inequality, labor market activity, insurance coverage, and health status, and provides a brief discussion of whether the favorable trends of the past half century can continue in the next few decades.
- The Transformation of Medicare, 2015 to 2030, Henry J. Aaron and Robert Reischauer: This paper discusses how Medicare can be made a better program and how it should look in 2030s using the perspectives of beneficiaries, policymakers and administrators; and that of society at large.
- Could Improving Choice and Competition in Medicare Advantage be the Future of Medicare?, Alice Rivlin and Willem Daniel: This paper explores the advantages and disadvantages of strengthening competition in Medicare Advantage (MA), including a look at the bidding process and replacing fee-for-service methodologies.
- Improving Provider Payment in Medicare, Paul Ginsburg and Gail Wilensky: This paper discusses the various alternative payment models currently being implemented in the private sector and elsewhere that can be employed in the Medicare program to preserve quality of care and also reduce costs.