TRACE
TRACE (Testing Responses through Agent-based Computational Epidemiology) is a collaborative effort by researchers from The Brookings Institution and Washington University in St. Louis to produce a sophisticated computational simulation model to inform policy responses to the COVID-19 pandemic in the United States. Results from our initial analysis with the model, and an interactive dashboard to allow direct engagement with the simulation outputs, are presented on this page.
Key Results
Below, we summarize six key results from our initial analysis with the TRACE model. Further detail related to each result can be accessed from the hyperlinks in each section.
1. Suppression is an attainable goal
Our model suggests that intervention strategies exist that can successfully suppress the spread of COVID-19 while lifting the mass-social distancing measures currently in place in much of the United States. Suppression means not just “flattening the curve” by spreading out infections over time, but ongoing containment that prevents sustained spread and a large number of new cases. A primary goal of TRACE is to identify policies that yield true suppression of the epidemic while gradually relaxing social distancing.
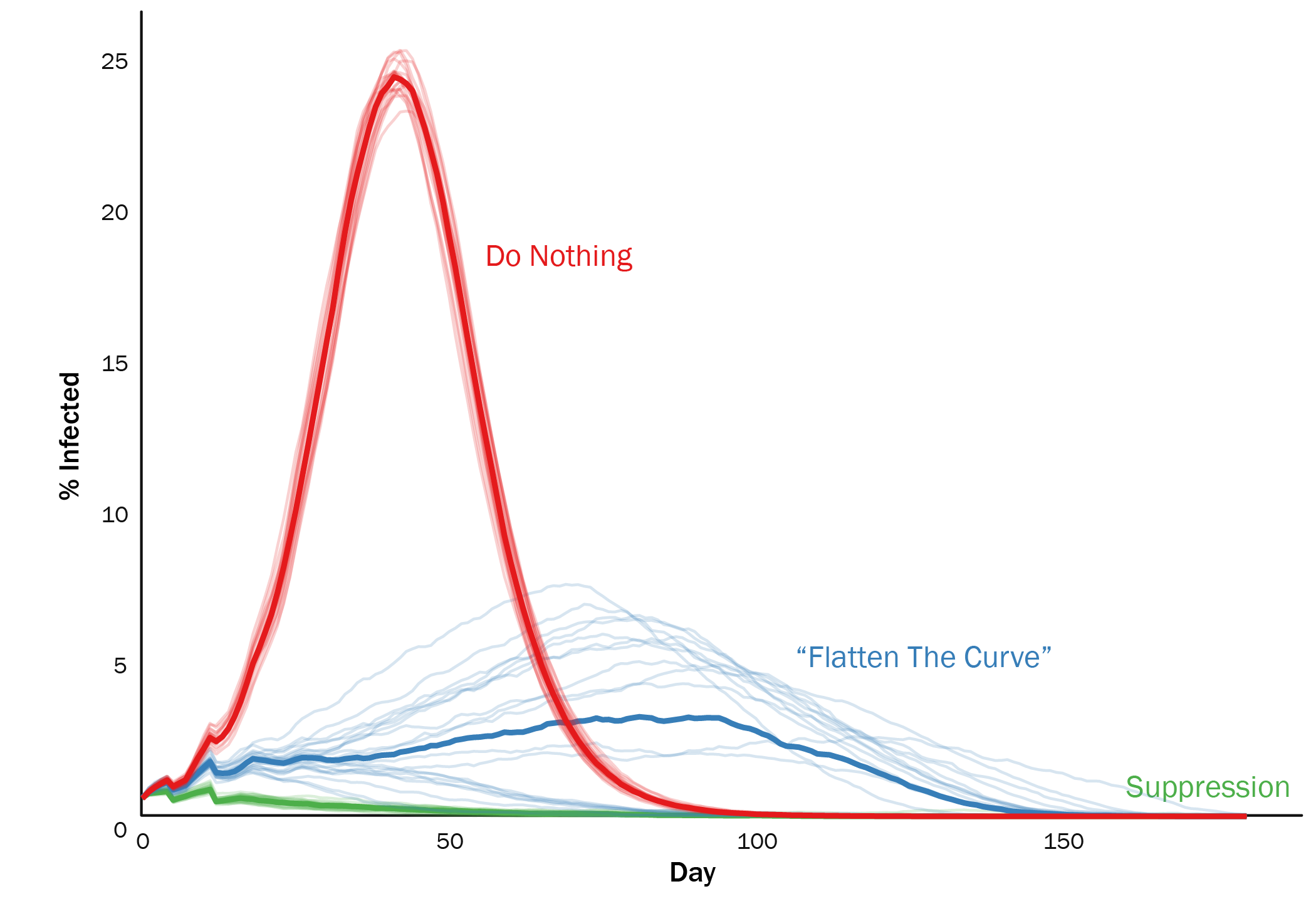 Figure 1. Relaxing social distancing with current national capacity for testing and contact tracing “flattens the curve” (blue curve). A more gradual relaxation of social distancing combined with expanded testing and quarantine policies can yield true suppression (green curve). In the absence of new infections from elsewhere, all three scenarios show cases eventually dropping to zero, but the cumulative burden of disease is much higher for the red and blue curves.
Figure 1. Relaxing social distancing with current national capacity for testing and contact tracing “flattens the curve” (blue curve). A more gradual relaxation of social distancing combined with expanded testing and quarantine policies can yield true suppression (green curve). In the absence of new infections from elsewhere, all three scenarios show cases eventually dropping to zero, but the cumulative burden of disease is much higher for the red and blue curves.
How test-and-trace policies are designed and implemented can matter a lot for success in containing epidemic spread. These choices include:
- how many tests of each type (PCR and serological) are available per day,
- how accurate they are,
- to whom they are given,
- what action is taken based on the results,
- and how much capacity there is for daily contact tracing.
Overall, we simulated a wide range of policy implementation scenarios (a total of 10,000 different options). Our simulations suggest that there are multiple ways to use testing-and-tracing to partially or fully substitute for shelter-in-place and other social distancing measures.
2. Policy should be robust to uncertainty
Broadly, there are two types of uncertainty facing policymakers using models as input into decision-making:
- Epidemiological Uncertainty about the underlying biology of the COVID-19 coronavirus and how it spreads
- Model Uncertainty: even for a single set of epidemiological assumptions, there may be a range of possible projected outcomes for a single policy (partly due to random chance reflecting natural variation across time and space in the real world, and partly due to modeling choices)
The specific policy choices that are most effective depend in part on underlying aspects of the epidemiology, many of which remain uncertain. These include:
- the baseline reproductive rate of the disease,
- the degree to which asymptomatic cases are capable of infecting others,
- how much background immunity has already been created in the population,
- and how many contagious individuals there are at the start of the new policy
We simulated how policies fared across a wide range of possible epidemiological scenarios, ranging from Most Unfavorable to Most Favorable. (See here for more details and definitions).
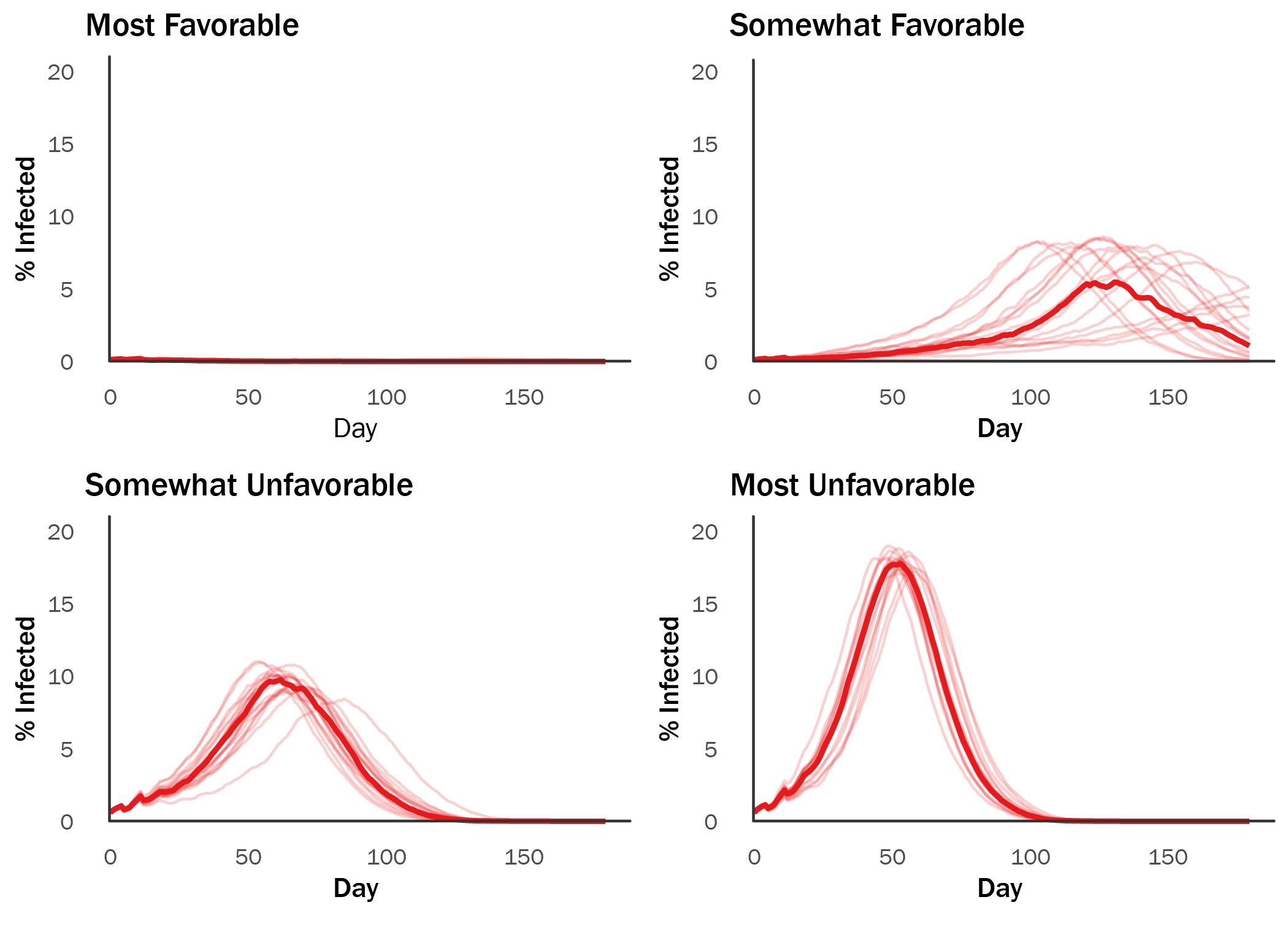 Figure 2. The same policy can yield multiple outcomes depending on underlying epidemiological parameters.
Figure 2. The same policy can yield multiple outcomes depending on underlying epidemiological parameters.
A robust policy response should take this uncertainty into account, and be designed to perform well even in the worst case projected scenario. (In all of the remaining result charts below, we assume the most unfavorable epidemiological parameters simulated).
3. Adherence is critical
As in the real world, agents in our model can choose to ignore social distancing or quarantine orders. For the policies we simulated, success or failure often depends critically on how people respond.
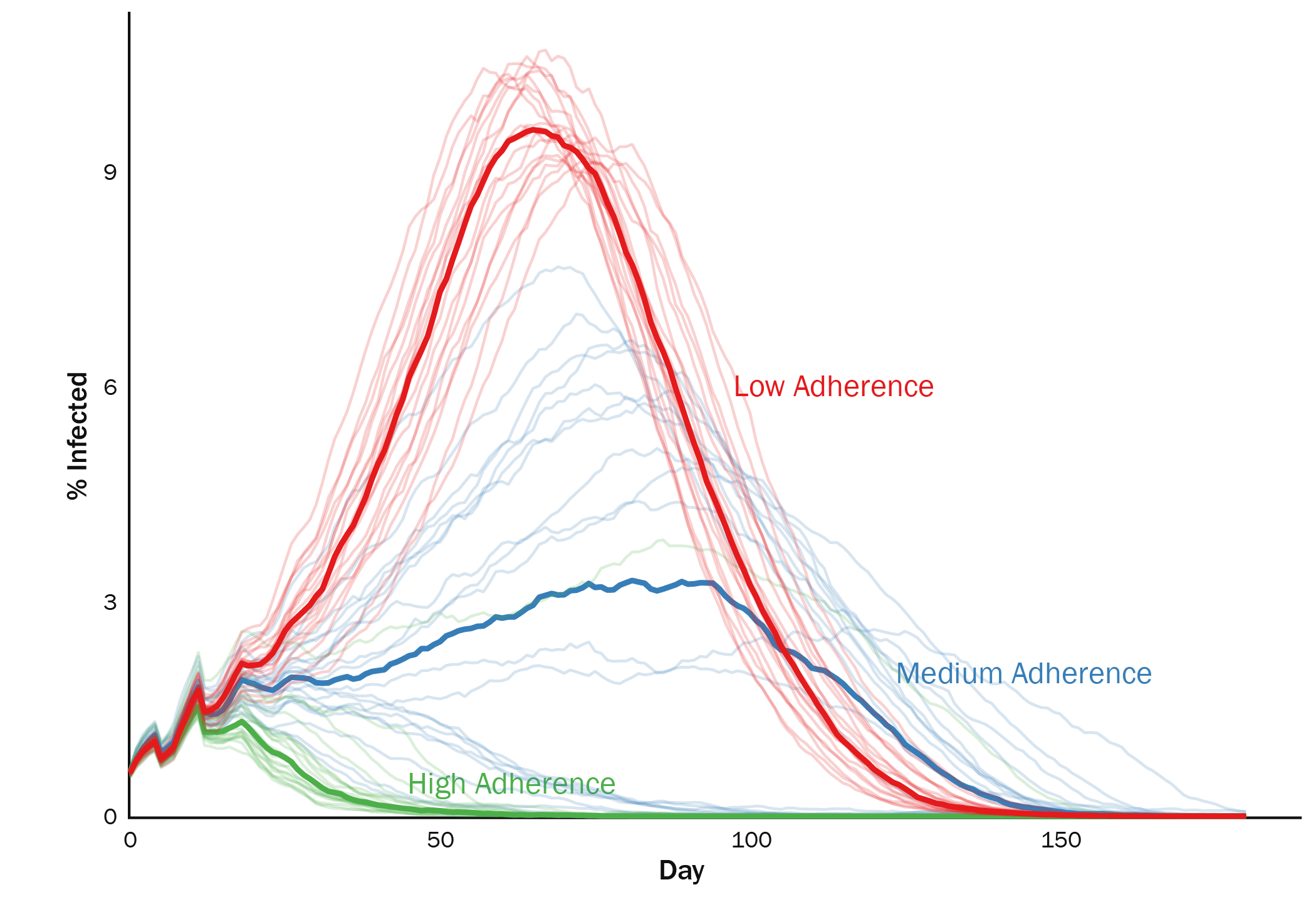 Figure 3. Low adherence can undermine any policy. Shown here is a policy that successfully suppresses the epidemic when adherence is high, but does poorly when adherence drops. A central aim of policy should thus be to encourage adherence through consistent, widespread messaging, and to make self-isolation financially and logistically feasible for any American if it becomes necessary.
Figure 3. Low adherence can undermine any policy. Shown here is a policy that successfully suppresses the epidemic when adherence is high, but does poorly when adherence drops. A central aim of policy should thus be to encourage adherence through consistent, widespread messaging, and to make self-isolation financially and logistically feasible for any American if it becomes necessary.
4. Gradually relax social distancing
The effective reproduction number of an epidemic (R) depends in part on the average number of close contacts that people have each day. The most effective policies continue to minimize these contacts even as other parts of the economy reopen.
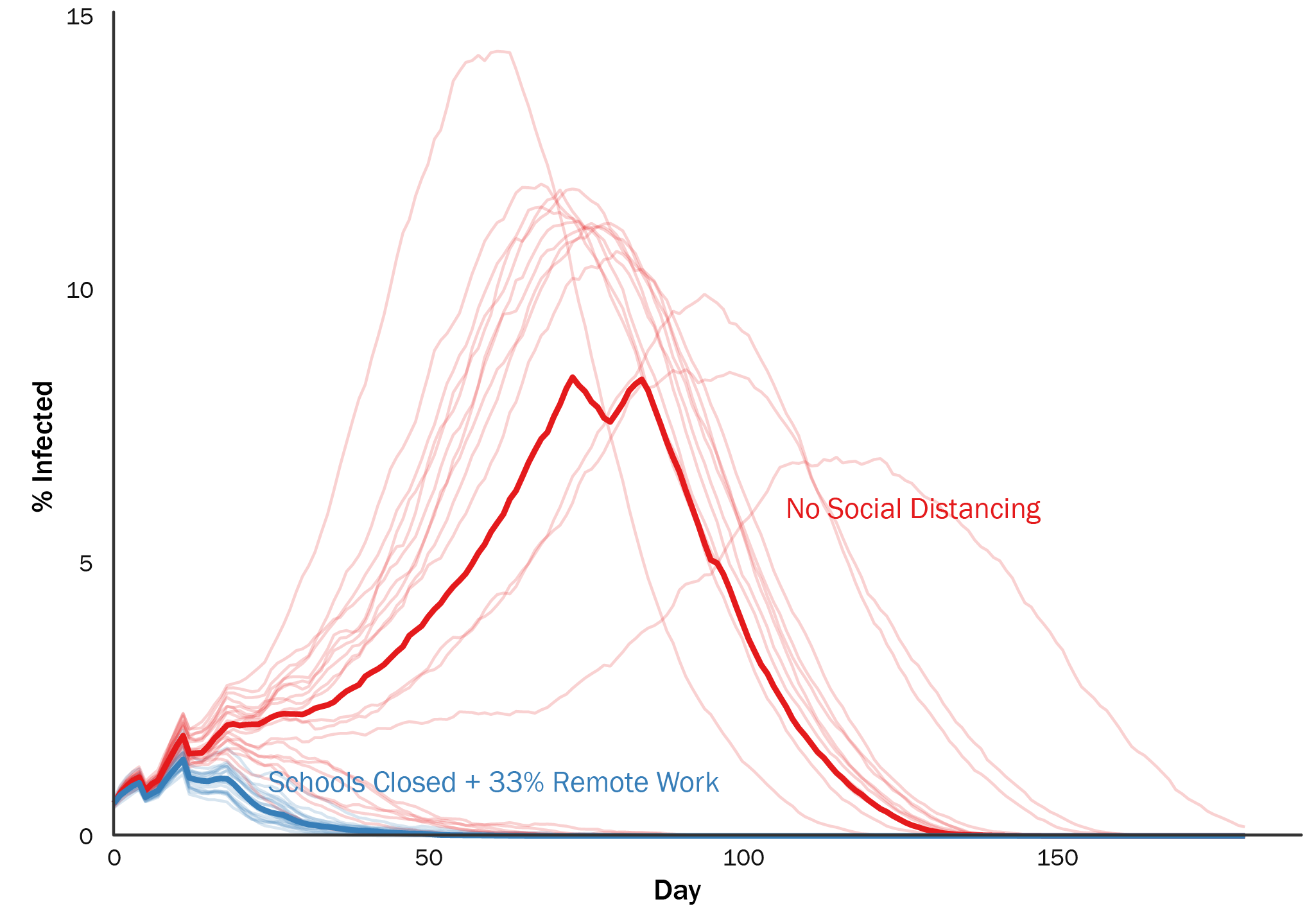 Figure 4. With limited capacity to test and trace infected individuals, maintaining temporary school closures and remote work for roughly 33% of workers strictly outperforms relaxing social distancing all at once.
Figure 4. With limited capacity to test and trace infected individuals, maintaining temporary school closures and remote work for roughly 33% of workers strictly outperforms relaxing social distancing all at once.
Waiting to release social distancing until the number of active infections has fallen significantly improves the chance that subsequent test-and-trace policies will be successful.
5. With limited testing capacity, do not prioritize symptomatics
Our current testing capacity is likely insufficient to suppress the epidemic if we continue targeting tests towards symptomatic individuals. Our simulations project that unless we can double the number of daily PCR tests available, a more effective strategy is to assume that symptomatic individuals are infected and ask them to self-isolate for two weeks, reserving tests for potential asymptomatic carriers and priority populations (seniors, healthcare workers, law enforcement, etc.) This result accords with calls from Paul Romer to “stop testing the wrong people”, but we find that this strategy can still work without mass testing millions of Americans per day.
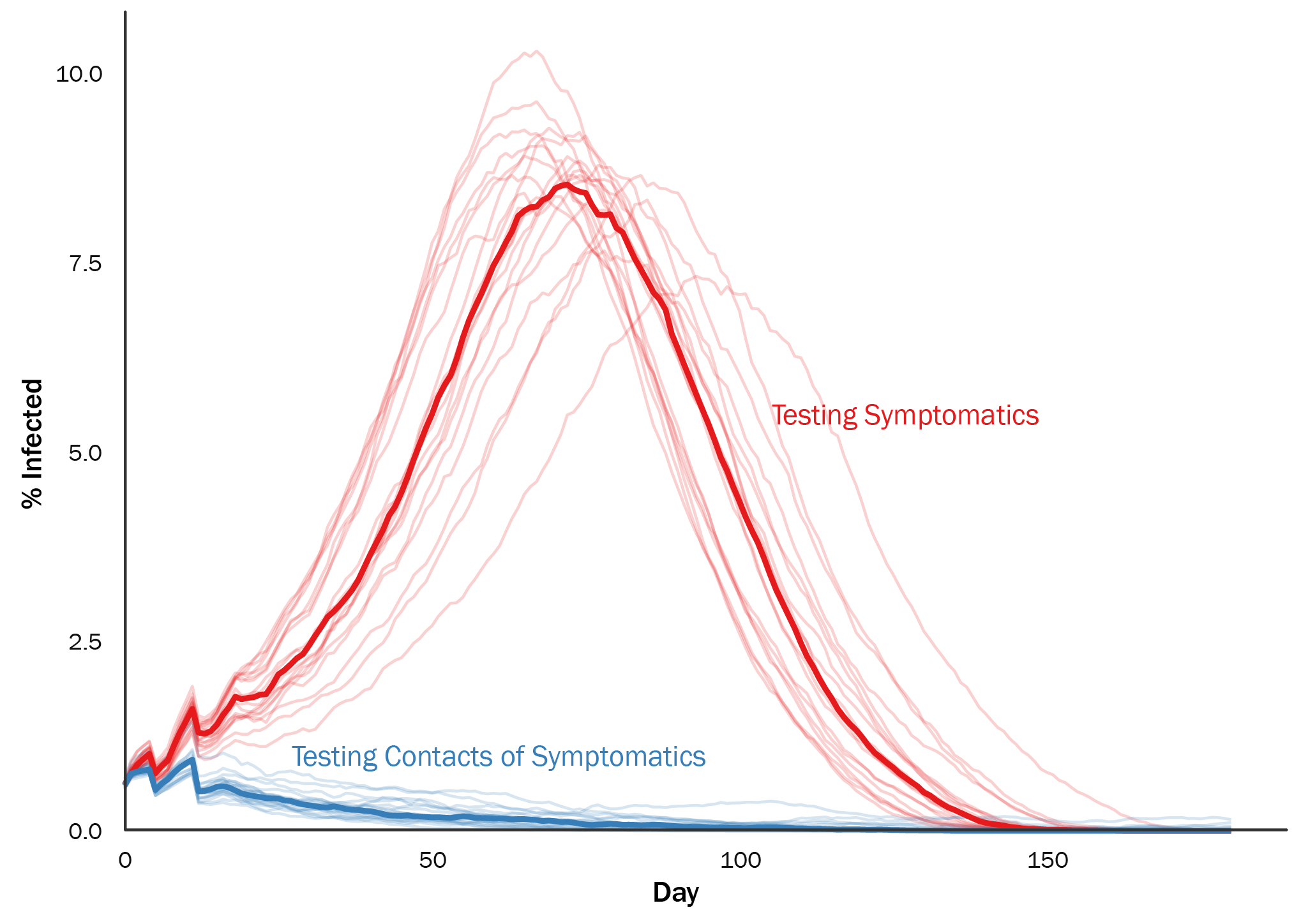 Figure 5. When testing capacity is low, prioritizing tests to contacts of symptomatic cases and asking symptomatic individuals to self-isolate significantly outperforms testing those with symptoms.
Figure 5. When testing capacity is low, prioritizing tests to contacts of symptomatic cases and asking symptomatic individuals to self-isolate significantly outperforms testing those with symptoms.
6. Mass serologic testing can help…but only if tests are accurate
One promising strategy involves combining PCR testing with serologic (antibody) tests. By identifying individuals who have unknowingly been exposed to the virus and freeing them from social distancing / quarantine orders, we can potentially free up the more limited PCR test capacity and minimize disruption by allowing those with potential immunity to get back to economic activities.
However, it has become clear that many existing serologic tests suffer from high false positive rates. Relying on these tests as part of a national strategy could backfire by clearing people as immune who are in fact susceptible or infected.
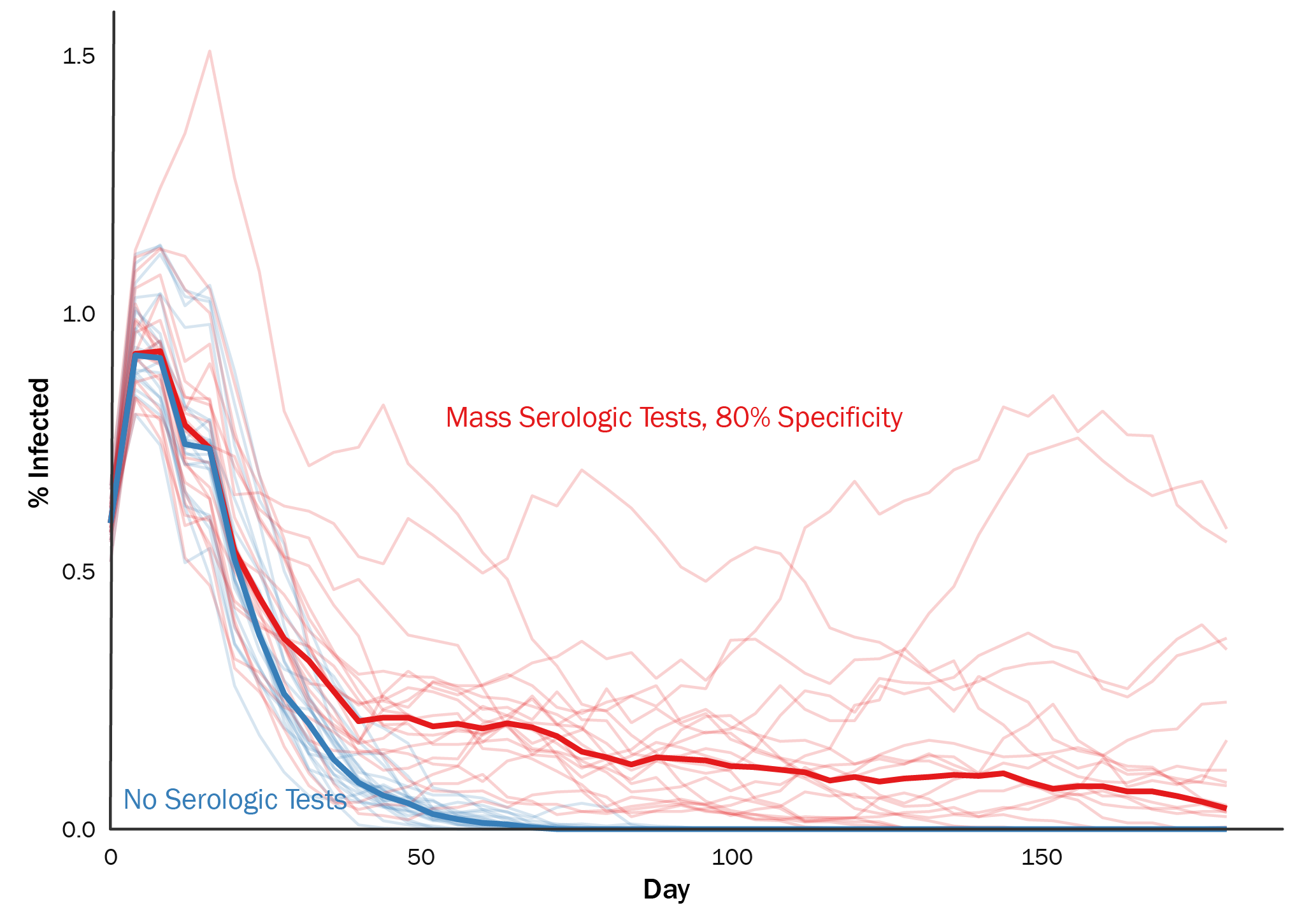 Figure 6. Highly inaccurate serologic tests can undermine successful policies by releasing susceptible individuals from social distancing too early.
Figure 6. Highly inaccurate serologic tests can undermine successful policies by releasing susceptible individuals from social distancing too early.