You can’t draw a straight line between growing Medicare spending and expanding American waistlines. But policymakers would be wise to keep both in mind as they ponder how to pay for the health care of 75-million-plus baby boomers who likely will live longer in worse health thanks to rising rates of chronic conditions, such as diabetes and heart disease, which in turn are fueled by growing obesity rates.
In a new report, we use the Future Elderly Model (FEM)—a microsimulation model of health and economic outcomes for older Americans—to generate a snapshot of changing Medicare demographics and spending between 2010 and 2030. During this period, the baby boomers, who began turning 65 and aging into Medicare in 2011, will drive Medicare demographic changes, swelling the estimated U.S. population aged 65 or older from 39.7 million to 67.0 million.
Characteristics of a Typical Elderly Medicare Beneficiary, 2010 v. 2030
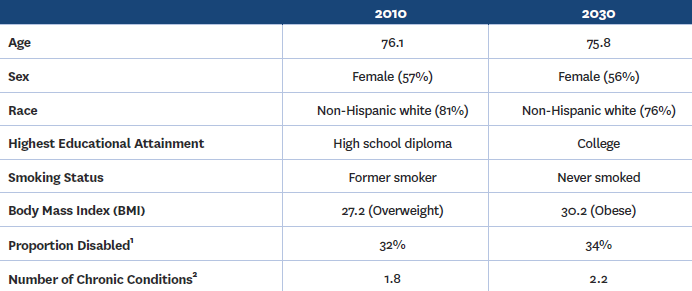
Generally, by 2030, the typical elderly Medicare beneficiary will continue to be female but slightly younger, less likely to be white, more educated, more likely to have never smoked but more likely to be disabled, obese and chronically ill.
In 2030, nearly one in two (47%) elderly Medicare beneficiaries will be obese, up from slightly more than one in four (28%) in 2010. In other words, obesity rates will increase about 1 percentage point a year during the 20-year period. Even more alarming, the share of people aged 65 or older with extreme obesity—defined as a body-mass index (BMI) of 40 kg/m2 or more—is expected to more than double between 2010 and 2030.
The prevalence of all major chronic conditions—high-blood pressure, heart disease, diabetes, cancer, stroke and lung disease—is expected to rise among elderly Medicare beneficiaries, driven by a combination of higher rates of obesity and gains in life expectancy. Diabetes is expected to grow the fastest, increasing from about one in four people aged 65 or older in 2010 to nearly four in 10 in 2030. Lung disease will see the slowest increase, from 15 percent in 2010 to 16 percent in 2030, largely because of declining smoking rates.
Fueled by these demographic and health shifts, the FEM predicts that Medicare spending will more than double to $1.2 trillion by 2030.
However, unforeseen medical innovation may greatly impact future outlays. As of now, most U.S. medical research, along with the health care delivery system, remains focused on disease-specific, acute, episodic illnesses. And while this disease-specific model has served the nation reasonably well to date, growing evidence suggests that it has not extended healthy life span for older people. Even when taking medical innovation into account the length of a healthy life span may well decrease in the coming years with chronic conditions on the rise.
At the same time, recent scientific advances suggest that slowing the aging process—known as senescence—might be possible. Delayed aging could be something akin to weight loss, which reduces the risk of many types of diseases simultaneously. We believe investing in this area of research should become a priority. That said, delayed-aging breakthroughs likely would allow more Americans to live long and prosper but also contribute to greater entitlement spending for older and healthier Americans down the road—we predict that such a development could add $295 billion to Medicare and Medicaid spending by 2060.
On the eve of Medicare’s 50th anniversary, it is clear that Medicare faces substantial fiscal risks. Among the risks, the size of the elderly population in the future likely will have the highest impact on spending but is easiest to forecast. Population health and the proportion of the future elderly with disabilities are more uncertain, though tools such as the Future Elderly Model—while not a crystal ball—can provide reasonable forecasts to guide policymakers. Finally, medical technology breakthroughs and their effect on longevity are most uncertain and perhaps riskiest. Policymakers will need to keep these risks in mind if we are to sustain Medicare for another 50 years.
Editor’s Note: Bryan Tysinger and Alwyn Cassil also contributed to this post. For additional information, download “Health and Health Care of Medicare Beneficiaries in 2030” a publication released at the half-day symposium, “Strengthening Medicare for 2030.”



Commentary
Medicare’s big fat problem, fiscal and otherwise
June 4, 2015