Background
![]()
To help support implementation of aligning clinical redesign with payment reforms in practices and institutions throughout the country, we present two cases from Duke University Health System (“Duke”) and University of Colorado Hospital (“Colorado”). The studies provide practical solutions for not only implementing clinical redesign, but also an understanding of how those clinical innovations can be aligned with alternative payment models. The cases will explore the following questions: What challenges or problems encouraged the organization to redesign CHF care? How did the organization select and then align care innovations with payment reforms, including bundled payments and shared savings? What did the organization identify as key success factors and/or challenges? How did these changes impact the organization׳s clinical outcomes or financial position? Finally, what lessons would the organization share with others attempting to implement similar strategies?
Personal Content
Living in the small southern town of Bristol, Tennessee at the age of 86, Robert Neelley Church takes deep pride in living an active life, especially after surviving a skin cancer diagnosis. But recently, Robert׳s health began to trouble him again. He developed chest pains and had difficulty breathing, putting a damper on his active lifestyle and routine activities. After consulting with his primary care physician, Robert was referred to a cardiologist to take a deeper look at his symptoms. After a few tests, Robert׳s cardiologist diagnosed him with mild congestive heart failure (CHF). After discussions with his physician and nurse about treatment and recovery options, Robert chose to have open heart surgery.
After surgery, Robert continued to experience persistent shortness of breath, even during mild physical exertion. A sudden worsening of symptoms almost took Robert to the emergency room, but instead his family encouraged him to go to the Duke University Health System׳s Same Day Access Heart Failure Clinic. While at the clinic, Robert met with his cardiologist, Dr. Zubin Eapen, and two nurses. Dr. Eapen spent time with Robert to help him understand what was happening to his heart and the rest of his body, and explained how additional treatments and behavior changes could help ease his symptoms.
A few days after their visits, Robert and his family were happy to see that his discomfort eased and his symptoms dissipated. But to this day, Robert and his friends and family play a significant role in managing and treating his chronic and challenging condition. Robert׳s story is just one of millions of Americans living with CHF in the United States.
Problem![]()
In this section, we will explore CHF’s clinical background.
Physiology and Symptoms
The average human heart beats four million times per year and pumps enough blood to fill a modern oil supertanker during a lifetime. However, over time some individuals may experience damage to cardiac muscles for a variety of reasons, such as plaque buildup in the arteries, heart attacks, or infections. This condition is known as congestive heart failure, a chronic disease with alternating periods of worsening and stability, with minimal recovery. Half of patients with CHF will die within five years of their diagnosis.1 Treatment often includes a number of medications and lifestyle modifications such as reduced sodium intake and daily physical activity. This unpredictable nature and variation in severity of symptoms significantly impacts the patient׳s use of health care services, the intensity of their care, and can often contribute to preventable hospital readmissions and mortality rates.
Epidemiology
CHF prevalence is highest in older patients, who make up a growing portion of the population (one in 5 Americans will be older than 65 years of age by 2050). Of all patients hospitalized with CHF, 75 percent are over the age of 65, and half are over 75. According to the American Heart Association, nearly 6 million Americans suffer from CHF, and an additional 555,000 are diagnosed each year. This chronic condition accounts for one million hospitalizations in the U.S. annually, and is the leading cause of hospitalization among adults over the age of 65.2 CHF accounts for a staggering 17 percent of overall national health expenditures, $273 billion in direct medical costs, and $172 billion in indirect costs.3,4
Many CHF patients also suffer from multiple illnesses or co-morbidities, often adding to the intensity of their care and treatment. Studies have shown that nearly 40 percent of CHF patients have five or more non-cardiac comorbidities, and account for 81 percent of the total CHF inpatient days.4 This added complexity of multiple diseases has major implications for providers, patients, and their caregivers and families that need to support them in their daily lives.
Solution![]()
Optimizing CHF care: prevent, manage and stabilize
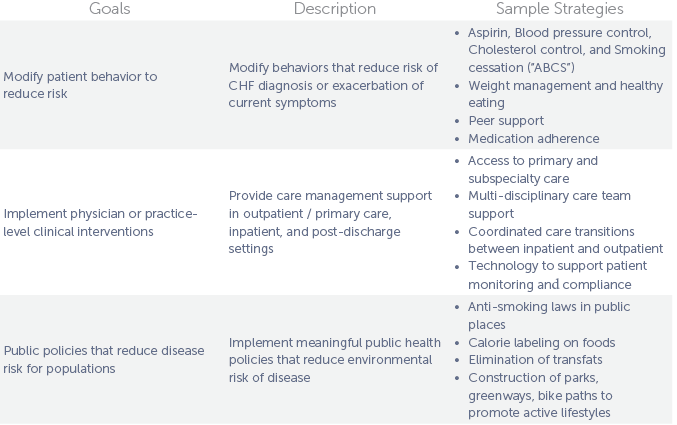
Clinical approaches to chronic disease management benefit from a three-pronged approach that addresses (1) patient behavior; (2) physician or practice-level clinical interventions; and (3) public policy or population health strategies (Fig. 1.)
Fig. 1. Three pronged optimal care approach
Payment Reform
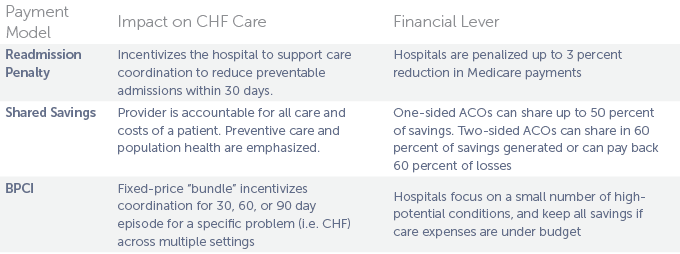
Medicare Readmission Reduction Program: In 2012 through the Affordable Care Act, Medicare began the Hospital Readmission Reduction Program, which levied penalties to hospitals with higher-than-expected rates of 30-day readmission after discharge.5
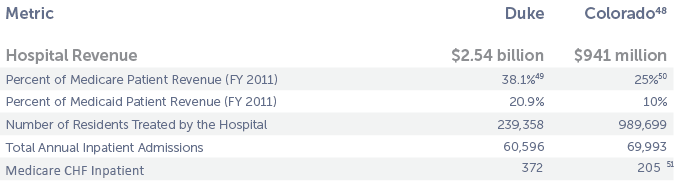
A hospital with a high proportion of patients readmitted within a short time frame could be an indication of poor quality of care in the hospital or a lack of appropriate coordination of post discharge care.6 It could also be an indication, particularly in an academic medical center setting, of a lesser opportunity to reduce preventable readmissions based on a higher acuity patient population. Based on a calculation of 2012 revenues and payer mix, Duke could be at risk for penalties up to $29 million and Colorado could face up to $7 million (though their rates currently do not merit penalties).
Alternative Payment Models: In 2013 the Center for Medicare and Medicaid Innovation (CMMI), a component of CMS, began offering enrollment in two optional programs. The programs, Bundled Payment for Care Improvement (BPCI) Initiative and the Accountable Care Organization (ACO)/Medicare Shared Savings Program (MSSP), were attractive to Duke and Colorado. Each posed specific risks and benefits, which ultimately resulted in different choices. Overall, each organization is dedicated to linking clinical innovations to payment reforms that encouraged a value-based system – one that rewards based on quality, outcomes, and reducing inefficiencies, such as preventable readmissions – as opposed to a volume-based system that is based on number of tests, procedures, etc. (Fig. 2).
Fig. 2. Financial impact and payment models in the context of CHF care
Organizational Context![]()
Duke University Health System: The Path to Accountable Care
Duke University Health System is a nonprofit, academic health care system comprised of Duke University School of Medicine, three hospitals, and several primary and specialty care clinics, home care, hospice, wellness centers, and community-based clinical partnerships.
Fig. 3. Duke and Colorado financial comparison metrics (FY2011)12, 13
The challenge of care redesign
In the 1990s, Dr. Christopher O׳Connor, a cardiologist, first explored challenges providers faced when trying to provide quality CHF care. These included (1) Poor coordination of care. Patients saw primary care physicians, cardiologists, surgeons, dieticians, social workers, and others, who often failed to communicate with each other, and only the patient was aware of all the appointments and tests. (2) No access to outpatient or primary care. Patients were unsure of whom to reach out to with questions or concerns, and did not always have access to providers at the exact time they required care. This fragmentation almost always resulted in unnecessary emergency room or hospital visits. (3) Inadequate disease information and guidelines. At the time, there was very little information about CHF disease management. Neither professional organizations nor trade groups had issued CHF treatment guidelines.
To address these challenges, Duke began a program of care improvement, with three major CHF initiatives that evolved over the next 15 years, including the Duke Heart Failure Program, the Heart@Home Initiative, and Same Day Access Clinic.
The Duke Heart Failure program
Dr. O’Connor received a $100,000 seed grant to create the Duke Heart Failure Program. The proposed strategy included, a geographically distinct unit for CHF, multidisciplinary care teams that included physicians (cardiology, family practice, and internists), nurses, dieticians, therapists, pharmacists, and administrative staff, formally defined care guidelines that identify patients based on New York Health Association (NYHA) functional classification, and an outpatient disease management clinic, which served as the foundation for the Same Day Access Clinic.
For patients enrolled in the program from July 1998 to April 1999, study data indicated the hospitalization rate decreased from 1.5 to 0 hospitalizations per patient per year while the number of clinic visits increased from 4.3 to 9.8 clinic visits per patient per year. Duke saved a median of $8571 in charges per patient per year as a result of reduced inpatient costs.7
Despite the fact that the program proved successful at reducing costs, there was no change in their contracts with payers. Fast forward ten years – in 2011, Dr. Zubin Eapen became involved in the CHF program leadership, and redoubled delivery reform efforts after Medicare instituted the Hospital Readmission Reduction Program in 2012.
Heart@Home Initiative
To become self-sustaining, the H@H team determined that preventing 1 readmission every 2 weeks would result in a 1percent reduction in total CHF case costs. This was calculated by determining the amount at risk due to the 3 percent Medicare Readmission penalty, nearly $30 million a year. The H@H financing model covers the costs of the program intervention and administration, with savings accruing to the payers (the total amount of savings is unknown at the time of publication).
In 2012, with encouragement from Duke Heart Center leadership such as Dr. Bimal Shah, Catherine McCarver, and others partnered with the Duke Translational Nursing Institute (DTNI) and Dr. Bradi Granger to obtain $500,000 in grants to fund further improvements. Specific changes included: (1) putting in place a dedicated care team for each patient, (2) improving communication, (3) coordinating care across all providers and sites of care, and creating standard protocols for post-discharge processes, including follow up procedures, ensuring all inpatients discharged from the hospital had an outpatient follow-up within 1 week, and (4) patient education and self-care support such as an iPad app, which captures specific CHF information that is exchanged with providers, including an interactive calendar, self-assessments, education modules, and an online pill box.
Same Day Access Clinic
Duke researchers analyzed an American Heart Association registry of thousands of Medicare patients, and found that seeing a doctor within seven days of a hospitalization significantly reduced the risk of readmission, emphasizing the need to improve post-discharge care. As a result, the leadership decided to launch a Same Day Access (SDA) Heart Failure clinic that would allow patients to see a CHF specialist immediately without an appointment. The SDA Clinic opened in 2012 and is located in the cardiology outpatient offices. This “one-stop shop” provides consistency of care, ensures proper transitions, and assists with navigating the health system and managing comorbidities.
Outcomes and Results
Preventable CHF readmission rates at Duke have gone down 15 percent in the first year of the initiative.8 Secondary clinical outcomes include improved quality of patient care transitions evaluated using measures of communication, patient satisfaction, and skill-based educational outcomes that include patients׳ ability to understand and manage medicines, symptoms, dietary salt intake, and daily activity.
Aligning Payment Reforms: The Shared Savings ACO Model![]()
Duke׳s physician leadership is committed to improving CHF delivery and had interest in exploring new payment models. Ultimately, the Duke care redesign team and senior leaders elected to enroll in the ACO MSSP. Launched in January 2014, Duke Connected Care, is a community-based, physician-led MSSP ACO that includes 1700 doctors from Duke, the Lincoln Community Health Center, and three other practices to care for a population of over 45,000 Medicare beneficiaries.
Why Duke Chose Not to Pursue a Bundled Payment for CHF
The economic principle behind a bundle is to separate technical risk (things clinicians can manage) from probability risks (things outside their control), and transfer the former to clinicians and the latter to insurers. Perhaps one of the most important factors driving Duke׳s decision is the inherent variability of CHF; they believe separating technical from probability risks in CHFwould be very difficult. Duke expressed concern that efforts aimed at decreasing admissions for CHF might, in a bundled payment, create financial incentives that were misaligned with the goals of improving patient care. Namely, a shift in volumes to higher-acuity CHF inpatients might over-emphasize probability risks compared to prior years. BPCI episodes typically fall into one of two categories-medical and surgical. Surgical episodes, such as a knee replacement, can be easier to predict and have less variability among the care needed. Medical episodes, particularly chronic, complex conditions like CHF, have a much greater range in care needed- both inpatient and outpatient, which is a key reason the bundles have not gained widespread traction. The variation in care leads to extremely high cost cases, that create risk for BPCI participants, while also creating potential opportunties for savings through improvements in care delivery.
Duke׳s leadership in particular believed that a variety of complicating factors in its patient population could make any bundle for CHF too risky. One of the greatest strengths of a bundle is to provide predictability and standardization of care and costs. Due to the complexity of CHF, medical and support care is not systematically applied the same way to each patient. Further, CHF is not an isolated acute care episode with a clear beginning and end that lends itself to developing a fixed payment per episode. In addition to the MSSP, Duke did enroll in one BPCI pilot: percutaneous cardiac intervention (a procedure used to treat narrowed arteries in a patient׳s heart, known as PCI) instead of CHF. This was a way of “dipping a toe in the water” until better metrics and risk adjustment can be developed for CHF based on experience managing the PCI bundle. Unlike a bundle that is procedure oriented with a well-defined start and episode of care, the chronic nature of CHF as a disease made an index hospitalization less appealing as a trigger for a bundled payment. Duke was also unsure if the BPCI׳s required 30, 60, or 90-day bundle would be appropriate for CHF because they hoped to focus on care strategies, such as Heart@Home, that went beyond these time periods to determine the stability of a discharged CHF patient.
Due to the variety of unknown factors involved, Duke took a conservative approach. Known CHF costs were indexed in the inpatient setting. Yet, a large portion of costs and care was performed in outpatient settings. Such longitudinal, post-acute care is often performed in rehabilitation centers, community health centers, and skilled nursing facilities that Duke does not have control over care and costs. They also did not have enough evidence that their clinical interventions were effective in reducing CHF costs. Thus, they worried that a large investment of resources in new delivery models was unlikely to result in significant cost reduction that would reap savings in a bundled payment setting. In contrast, Duke׳s participation in the MSSP program will, in the long term, lead to investment in enhanced primary care services. This may lead to more fundamental delivery reform and potential investments in prevention and population health.
University of Colorado Hospital: The Path to Bundled Payments![]()
The University of Colorado Hospital is an academic medical center composed of four campuses and five hospitals across the state based in Aurora, CO. The three major components of the system are the hospitals, the School of Medicine, and United Physicians Inc. (UPI), a nonprofit organization that supports the medical operations of Colorado. Elizabeth Kissick, the director of health plan development for UPI and Dr. Larry Allen, a professor and cardiologist have been administrative and clinical leaders in the push toward care and payment redesign, especially for the CHF population.
The Challenge of Care Redesign
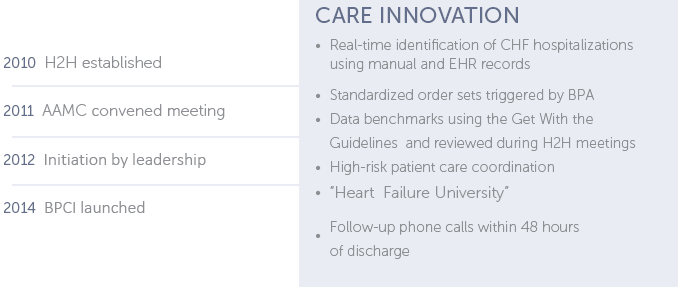
The American College of Cardiology and Institute for Healthcare Improvement started the national “Hospital to Home,” or H2H program. This program is a resource for hospitals and cardiovascular care providers committed to improving transitions from hospital to “home” and reduce their risk of readmission penalties.9 In 2010, Dr. Larry Allen, an advanced CHF and transplant physician, identified a need at his own hospital, and started a Colorado-based H2H in 2010. Like Duke, Colorado has re-engineered its care of CHF, but with a very specific focus on using technological innovation to reduce length of inpatient hospitalizations and reduce readmissions (Fig. 4).
Fig. 4. Colorado heart failure innovation timeline
Choosing bundled payments
The team at Colorado prepared an environmental analysis of payment reform, and for a number of years, was engaged in a number of Colorado state initiatives for state-wide bundling in Medicaid and the private sector. Colorado viewed the model as an expansion of a previous demonstration model – this familiarity with the payment model and evidence of cost savings helped minimize the associated risks. Ms. Kissick worked with the American Association of Medical Colleges (AAMC), a convener under contract from Medicare to assist with pilot participation, to create a program to begin in January 2014.
Under the BPCI, participants had the option to choose from one of four models; Colorado chose a 30-day, model 4 bundle. This model utilized prospective payments such that the hospital would receive a single, lump sum payment from Medicare and then distribute that payment among all of the providers involved in the episode of care – and if their costs exceed the budget, Colorado would absorb the extra costs. When compared to fellow BPCI participants, 116 institutions implemented a CHF bundle, with Colorado being the only institution to opt for a 30-day model; others all chose longer time periods (60–90 days).
BPCI makes hospitals financially responsible for services provided if a readmission occurs. For example, CMS would not pay claims for CHF related services provided at Colorado within 30 days of the anchor hospitalization. In addition, for any CHF-related services provided at another hospital, Colorado would be financially responsible for the total payments made during that readmission.10
Colorado felt that the 30 day bundle was the best option because it allows hospitals to begin taking risk for acute-care services, while they ready themselves to take accountability for post-acute care services and hospital readmissions. It also sets the stage to work toward a fixed budget with the prospective payments – something that will become commonplace sooner rather than later.11 Colorado only projected an approximate $40,000 savings in the first year of the BPCI. This amount would cover the discount to CMS and other costs such as the investment made for data discovery and costs associated with preparing the application. This small amount relative to overall Colorado revenue, illustrated Colorado׳s commitment to reform payment despite a small incentive.
Colorado customized the bundle and gain-sharing structure that would accommodate their provider expertise, interest, service mix, and patient population. Colorado proposed which Medicare services were included and excluded in the bundle. Colorado estimated that there would be about 100 Medicare patients who would be discharged with primary diagnosis of heart failure (based on prior data).
Solution and Key Lessons
![]()
There were a number of factors present at both institutions that were critical to the success of their projects that may be helpful for other organizations interested in implementing these clinical and financing reforms.
A commitment to continuous improvement in large centers can flourish in the presence of initially small financial incentives. Both centers made significant steps to improve care quality even in areas where significant financial gains were not expected (for example, the upside for Colorado was less than $40,000 per year).
Impact of “demand destruction” on financial risk-taking. With better care coordination, hospital healthcare spending will be reduced as a result of decreased volume, and this can have a negative impact on those hospitals׳ operating margins. Therefore, bundled payments may not be the best option over long periods, if the organization cannot adapt their business model to accommodate the decrease in revenue.
Clinical leadership is essential to change management and quality improvement. Duke and Colorado have highly committed clinical leaders who envisioned and pursued innovative care. The effect of top-down leadership is essential in supporting a commitment to continuous quality improvement and a culture of learning and innovation.
Convening organizations play a key role in providing technical assistance and implementation support. Clinical leaders and health systems do not always have a complete set of tools for payment reform. Thus, conveners contracted by CMMI, played a helpful role in catalyzing payment reform for their members.
The future of further care redesign is uncertain. While both organizations began with relatively small-scale, incremental pilot programs around CHF, it remains to be seen if this will lead to broader redesign of CHF care. While such changes can be incentivized by shared savings ACOs or bundled payments, time will tell if the centers pursue more comprehensive, high-value changes in care.
Policy Recommendations![]()
Create more direct clinician incentives for quality-related outcomes. For such small changes to lead to larger ones, clinicians must be rewarded or penalized with clearer connections to clinical outcomes under their control. This would require the creation of numerous financial “microenvironments” through a large organization (for example, with partially bundled payments), with well-designed supportive electronic medical records. This must include start-up costs for upfront changes in infrastructure.
Improve coordination and best-practice sharing between various institutions. Though clinical leaders and hospitals each pursued innovations in care, hospitals appeared to work in isolation without clear standardization or sharing of best practices.
Improve long-term incentives for clinical leaders. A key component of sustainability is to provide meaningful recognition to such clinician leaders in academic and other settings. In addition, clinicians could perhaps satisfy licensing or board certification requirements with direct, meaningful involvement in delivery reform. Such innovative uses of recertification might create broader interest in clinical redesign and payment reform.
Rethink existing value-based purchasing (VBP) and pay-for-performance programs. Neither Duke nor Colorado clinical leaders reported that these initiatives encouraged strongly enough the kind of global care redesign that might lead to additional opportunties for improvement in meaningful long-term outcomes. A consolidation of the VBP program at some point into the BPCI or Shared Savings models would be beneficial.
Establish long-term funding for technical assistance and startup costs. Though convening organization played an important role in seeding CMMI pilot programs, no long-term, continuing sources of funding are present. Additionally, these conveners could expand to cover not only Medicare pilot programs, but also help design programs targeting and consolidating a health system׳s private insurers into such pilots as well, to create amplified, focused incentives.
Prioritize simplicity in payment reforms. Perhaps future rounds of reforms could consider partial bundles for certain episodes, which are administratively simpler (for example, like hospital DRGs), and also do not depend on highly complex and labor intensive analysis. Measures could also be considered to cap total regulatory and reporting burdens to reasonable levels.
Acknowledgment: The authors thank Dr. Richard Merkin and the Merkin Family Foundation for their support of this publication, and for supporting the Engelberg Center for Health Care Reform׳s efforts in policy leadership around innovations in care delivery and payment reform.
References
1 C. Yancy et al. AACF/AHA guideline for the management of heart failure. Circulation, 128 (2013), pp. 240–327.
2 Ibid.
3 Ibid.
4 Prospective Payment Systems for Inpatient Hospital Services, 412 C.F.R. §412.150 to §412.154 (2012).
5 J. James. Medicare hospital readmissions reduction program. Health Aff, 33 (3) (2013)
6 Ibid.
7 Adrian F Hernandez et al. Relationship between early physician follow up and 30 day readmission among Medicare beneficiaries hospitalized for heart failure. J Am Med Assoc, 303 (17) (2010), pp. 1716–1722.
8 Duke Translational Medicine Institute.
Same-day access heart failure clinic provides inter-disciplinary research opportunities
. (2013, September).
9 Quality Improvement for Institutions. (n.d.).
Hospital to home
.
10 Center for Medicare & Medicaid Innovation.
Bundled payments for care improvement initiative (BPCI) background on model 4 for prospective participants
. (2014, February).
11 Herman B.
The advantages and disadvantages of CMS׳ bundled payment initiative: 8 responses
. Becker’s Hospital Review. (2011, October 07).
12 These numbers represent the entire Colorado system.
13 Brown, L.
Duke eye center expansion
. (2012, January 20).



Commentary
Case Study: Delivery and Payment Reform in Congestive Heart Failure at Two Large Academic Centers
May 9, 2014