This brief is part of the Brookings Blueprints for American Renewal & Prosperity project.
Despair in our society is a barrier to reviving our labor markets and productivity, jeopardizes our well-being, health, and longevity, and affects our politics. Despair was increasing among Americans well before COVID-19; the virus was an exponential shock.
Before the virus, the U.S. boasted robust stock-markets and record low levels of unemployment, yet 20% of prime-aged males were out of the labor force.1 From 2005 to 2019, an average of 70,000 Americans died annually from deaths of despair (suicide, drug overdose, and alcohol poisoning). These deaths are concentrated among less than college educated middle-aged whites, with the those out of the labor force disproportionately represented.2 Low-income minorities are significantly more optimistic than whites and much less likely to die of these deaths.
This despair reflects the decline of the white working class. It contributes to our decreasing geographic mobility,3 and has political spillovers. Counties with more respondents reporting lost hope in the years before 2016 were more likely to vote for Trump.4
Policy responses have been fragmented, with most focus on drug interdiction rather than on the root cause of despair. Even the public health efforts devoted to the problem do not have a strategy to address these. There are local efforts to boost the well-being of vulnerable cohorts, but most are isolated silos. There is no federal-level entity to provide financial or logistical support, nor is there a system that can disseminate relevant information to other communities seeking solutions. While federal agencies—such as the Centers for Disease Control and Prevention—track mortality trends, there is no system that tracks the underlying causes of these deaths. Our research has shown that significant drops in hope among less-educated white males preceded deaths of despair by several decades.5 Had we been measuring well-being regularly we could have helped avert a crisis of premature mortality.
This brief argues that the Biden administration ought to form a new federal interagency task force to address addiction and despair as a critical first step. This task force would monitor trends and coordinate federal efforts. Otherwise the large cohort of workers that have simply dropped out of the labor force and have lost hope of having a purposeful existence will continue to suffer and remain a barrier to a full economic recovery.
Challenge
The problem is a crisis of despair and associated premature death among significant parts of our population. Our challenge is how to reduce despair in places and populations where hope has been lost? This is not a traditional policy problem. Yet failing to address it will jeopardize our labor markets, productivity, and the much-needed post-COVID-19 recovery; shorten our life spans; exacerbate social and health problems; and poison our politics. Yet despite the tragic statistics, there are remarkable pockets of hope we can look to and learn from.
Lack of hope is a central issue. The American dream is in tatters and, ironically, it is worse for whites.6 The U.S. has higher levels of well-being differences across the rich and the poor than most wealthy countries and Latin America. Americans report more pain than respondents in 30 other wealthy countries.7 Whites, and particularly poor rural ones, report more pain than poor minorities, and America’s high levels of reported pain are largely driven by middle-aged whites. As there is no objective reason that whites should have more pain than minorities, who typically have significantly worse working conditions and access to health care, this suggests psychological pain as well as physical pain.
In addition to the economic and health shocks from COVID-19, the despair among the white working class drives nativist politics, vulnerability to fake news, populist messages, and skepticism about science. Those trends are even evident in response to and compliance with COVID-19 policies, with whites in general the group that is least likely to wear masks, as we find in the new COVID-19 survey (discussed below). Sadly, our society’s despair is even a factor in the ideological polarization that is hampering our response to a deadly pandemic.
There are a number of historical instances in which relative deprivation and insecurity about the future have led to support for extremist politicians (such as Weimar Germany); other recent work documents the links between financial crises (distinct from recessions) and extreme right wing voting in European countries over the past century.8 The tragic events at the Capitol on January 6—with additional instigation from others such as the president and a few legislators—are reminiscent. We will not emerge from it as a healthy and productive society unless we begin to address its root causes.
Prior to COVID-19, an average of 70,000 Americans died annually due to deaths of despair (suicides, overdoses, and alcohol-related illnesses). The rate of increase is also remarkable; while just under 20,000 people died of overdose in 2010, almost 75,000 did in 2017. Overdoses kill more Americans than suicides, motor vehicle accidents, firearms, and homicides; overdose is now a key contributor to the drop in Americans’ life expectancy.
Since COVID-19, death rates due to overdose have risen significantly, due to increased social isolation and joblessness (discussed in detail below). This crisis cannot be solved by simply reducing the supply of drugs. People in despair will inevitably find substitute drugs. Most recently, increasing numbers of individuals with substance use disorders have switched to illegal and more deadly opioid strands such as fentanyl, which is responsible for an increase in overdose deaths nationwide since 2017.9
There are long-term reasons for this. As blue-collar jobs began to decline from the late 1970s on, those displaced workers—and their—communities lost their purpose and identity and lack a narrative for going forward. For decades, whites had privileged access to these jobs and the stable communities that came with them. As globalization led companies to relocate elsewhere, many communities experienced high levels of joblessness, affecting marriages, unions, and civic organizations.10
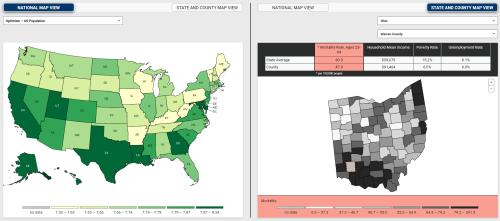
Primarily white manufacturing and mining communities—in the suburbs and rural areas and often in the heartland—have the highest rates of despair and deaths. In contrast, more diverse urban communities have higher levels of optimism, better health indicators, and significantly lower rates of these deaths. We have developed a vulnerability indicator that tracks—and visualizes—these trends in well-being and the linkages to deaths of despair and excess deaths due to COVID-19, highlighting the places in the country that are most vulnerable.
White men out of the labor force, meanwhile, have the worst health markers in the country, including high levels of opioid addiction and reported pain, and the lowest levels of hope compared to any labor market cohort. They are also much less likely to move to look for jobs. They tend to live in counties where a high percentage of respondents still live in their parents’ census tracts or homes. These counties tend to be the same ones that have experienced significant economic decline. The national average percentage of respondents that live in their parents’ census tract, per county, is 26.1, while the maximum level is 61.7—a large divergence across counties and regions. The average percent of respondents living in their parent’s homes as adults is 11.8, while the maximum is 42.9, again reflecting big differences across counties as well as the lack of mobility of the those out of the labor force, who tend to live in the high percentage counties.11
The lasting belief in the rewards to individual effort has also eroded in this group, while lack of trust in public safety nets remains. Skepticism of higher education and science leaves them more ill-equipped to navigate a future in which the nature of work—and particularly low-skilled jobs—is changing. High levels of addiction and despair in many of these communities is preclusive to moving to where the jobs are.12
In contrast, minorities, who had unequal access to those jobs and worse objective conditions to begin with, developed coping skills and supportive community ties in the absence of coherent public safety nets. Belief in education and strong communities have served them well in overcoming much adversity. African Americans remain more likely to believe in the value of a college education than are low-income whites.13 Minority communities based in part on having empathy for those who fall behind, meanwhile, have emerged from battling persistent discrimination.
Low-income whites remain skeptical of higher education, in part because it was not necessary to attain a stable, blue-collar lifestyle in the past. In contrast low-income Blacks continue to believe in it as an upward path and have been narrowing education gaps with whites over the past decades.14 In keeping with that trend, our ongoing surveys of the hopes and aspirations of young adolescents in low-income neighborhoods in Missouri are showing that conditional on graduating high school, low-income minorities are more likely to pursue college than their white counterparts.
Johns Hopkins sociologist Andrew Cherlin recently studied the children of former Bethlehem Steel workers in Baltimore.15 The mills, long since shuttered, were an anchor of the city’s blue-collar jobs. The Black workers were recruited from the South in the 1950s, lived in segregated housing, and faced constant discrimination in the workplace. Yet most of their children attended college and left Dundalk, the neighborhood surrounding the mills, for better parts of town. Yet in keeping with the role of communities of empathy, they come back weekly to the local church to give back. The children of the white workers largely remained in Dundalk, did not attend college, and work in the gig economy. This example is a microcosm of the broader patterns of minority optimism for the future and related investments compared to the relative decline—and lack of intergenerational or geographic mobility—of low-income whites.
Pain is a gateway into opioid addiction, meanwhile, and the lower likelihood that minorities are prescribed opioids ironically may have played a protective role. The vast increase of opioid prescriptions in the 2000s created a perfect storm. At the time that the medical community began to prioritize pain, opioid manufacturers such as Purdue Pharma began targeting the same declining blue-collar communities (where manual labor and pain often coincide), and adequate regulation lagged for decades. The so-called “pill-mill” towns in West Virginia and Kentucky are noteworthy, and those two states have among the highest levels of deaths of despair today.
The COVID-19 shock
The entrance of COVID-19 pushed this crisis to an entirely new level. While initially COVID-19 hit low-income minorities in big cities the most, this changed with the nationwide spread of the virus by fall of 2020, and its reach to rural areas in the heartland that already had high levels of deaths of despair, poor underlying health conditions, and years of decline in the availability of accessible hospitals and health care. While population density is lower in these places, the COVID-19 mortality rate is very high in many of them (see our interactive—cited above). The preexisting low levels of well-being and mental health increased the vulnerability of these populations.
The stress and anxiety surrounding COVID-19 and the isolation caused by necessary lockdown policies has exacerbated vulnerabilities everywhere, and surely in these hard-hit isolated places. While the economic shocks from the virus may be felt less in places where there are fewer industries left to fail, the other uncertainties caused by the virus also affect mental health. Concerns about eviction and job loss, and the loss of existing community support—no matter how minimal—contribute to more isolation and despair among already vulnerable people and add new ones to the ranks.
Finally, an unintended outcome of the CARES Act’s income transfers is an increase in opioid and other overdose rates as a result of people with substance use disorders using their cash to purchase drugs.16 At the same time, lockdowns and the virus make it much more difficult for EMS and other responders to get at-risk patients into treatment and make it much harder time to follow their progress over time. The spillover effects of these trends will be long-term. One of these is the increase in anxiety, depression, and suicide among the young, who are hit particularly hard by the lack of social contact and face an abysmal job market. Lack of hope and uncertainty about the future is a driving issue.
The results that we have to date are stark. New first responder data from the National EMS Information System (NEMSIS) shows significant increases in mental distress, overdose rates, and suicides. Mental health and overdose calls to first responders have doubled in 2020 compared to both 2018 and 2019 (Figures 1-2). Suicides have seen an uptick also, but at a lower rate (Figure 3)



Our new well-being data from surveys conducted during COVID-19, in collaboration with the Social Policy School at Washington University in Saint Louis, also show overall declines in mental health, drops in hope, and increases in anxiety. Remarkably, though, low-income Blacks remain the most optimistic low-income race cohort, even though they are the most at risk from COVID-19. They have experienced increases in anxiety, but their levels remain lower than those of other cohorts, and they report the lowest levels of loneliness and hopelessness. They also report feeling more worthwhile than any other cohort, especially whites (Figures 4-5). It seems that the same optimism and resilience that has helped African Americans cope with a history of adversity is also protective of mental health during the pandemic.


Limits of historic and existing policies
Past policies have focused largely on interdicting the supply of illegal drugs, which is a worthy cause but will not solve the demand problem. And even in the interdiction and tracking process, there is a lack of coordination between the many efforts, and a lack of connection to those concerned with the health effects of the opioid crisis. The Office of National Drug Control Policy, for example, coordinates several important tracking efforts, such as NEMSIS (cited above) and the Overdose Detection Mapping Application Program. The Substance Abuse and Mental Health Services Administration (SAMHSA) does important work supporting research and tracking of suicides and other mental health illnesses, but this is not connected with the interdiction efforts. There is no shortage of committed people and agencies, but there is no coordinating body that connects drug supply and demand problems with trends in the causes of despair, and especially economic decline. We need a coordinating body that connects those dealing directly with deaths of despair with those that are trying to deal with some of the root causes of the despair—including the decline of blue-collar jobs and the communities that used to support them. The intertwined problems of working class decline and the increase in despair and death among the same cohorts should be treated as a conjoined national priority, not in separate silos.
There has been progress on curtailing opioid prescribing practices, introducing new regulations, and prosecuting the companies that aggressively marketed these medicines in declining manufacturing and mining communities. Still, as noted above, that will not prevent already addicted people from switching from opioids to fentanyl, methadone, or any other drug that they can access.
More generally, there has also been a historical lack of attention to rural communities, which suffer from poor-quality education and health care, little access to broadband internet, and low civic participation among youth.17 They often also lack the institutions and capacity to take advantage of existing state or federal resources. These trends have helped drive the decline in civic trust, belief in education and science, and other trends that hamper any effective response to COVID-19 and to a recovery of our nation’s economic productivity, health, and well-being.
Policy recommendations
Reducing despair and its impact on our society’s health, longevity, well-being, and productivity is a complex, multifaceted problem that one policy alone cannot solve. It will require many approaches—some we know about and others that still need to be developed. As a necessary first step, the Biden administration ought to establish a White House coordinating body or interagency task force that can provide logistical assistance and modest financial support to ongoing local efforts in deprived communities, as well as to better coordinate federal programs, such as in drug interdiction, that can bolster and scale local responses.[i] Another role for the task force would be to marshal the use of tools such as our vulnerability indicator (discussed above) that provide information on where high levels of despair and economic decline intersect and reflect in the highest rates of mortality. Federal agencies, like Health and Human Services, Education, Labor, Commerce/Economic Development, and place-based agencies like Housing and Urban Development and the Department of Agriculture, would be natural members of this coordinated effort.
We have many examples of successful efforts to build from—both within and outside the U.S.—including specific interventions that enhance the well-being of the isolated and desperate. Like well-being interventions, economic efforts to help revive deprived communities must be local and tailored to specific communities. Yet they also stand to gain a lot from the logistical support that could come from an agency or task force that serves as an information clearinghouse for local practitioners trying to learn from their counterparts in other states and counties.
Success stories to build from
Addressing societal despair is not a usual policy challenge, nor are there magic bullet solutions. Yet there are successful initiatives that we can learn and build from and that can serve as a benchmark a coordinating agency could use to launch the process. Many countries around the world—such as the U.K. and New Zealand—have already made well-being a central policy priority, including using metrics of well-being in their official statistics as tools to assess budget priorities and the effects of policies to improve quality of life at the workplace or in health practices (including mental health)—thereby enhancing productivity, the effects of changes in environmental policies, and more.
Key to the success of these efforts has been one or more high-level government officials making a strong commitment to the effort. In the U.K., Lord Gus O’Donnell, former chief of cabinet under Brown, Blair, and Cameron, championed the cause of well-being, from getting the metrics into the official statistics to making it a national government priority. Lord Richard Layard, meanwhile, former minister of labor, led the charge to make mental health a priority, via the creation of a Ministry of Loneliness and an initiative for broader use of cognitive and behavioral therapy (CBT) to help combat depression. In New Zealand, Prime Minister Jacinda Arden has been a major driver of well-being as a national priority and the Ministry of the Treasury has been the primary implementing organization, placing it in a critical government agency and signaling that it is part of mainstream policy.
The British government also uses the metrics to design and evaluate policy interventions to enhance well-being in deprived or isolated populations or communities, via the What Works Wellbeing Centre, which receives both government and nongovernment support to operate. The Centre supports academic scholars to design and implement the interventions, and then has them independently evaluated for cost-effectiveness (both in income and well-being terms).18 The interventions are, for the most part, inexpensive and intuitive, but yield important improvements in well-being. These include increasing public participation in the arts, volunteering, and/or community environmental improvement programs (especially for isolated individuals), to interventions that seek to improve quality of life in the workplace, to training programs for underprivileged youth.
There are also examples of successful efforts in the U.S., although they tend to be local. The city of Santa Monica, for example, with initial support from a grant from Bloomberg Philanthropies and based on the advice from an expert panel of scholars in the field, implemented the first annual well-being survey in the United States, and for several years used the outcomes to frame municipal policy priorities. These included reducing the isolation and loneliness of low-income minorities via community-sponsored activities, such as group walks, involvement of local youth in art projects designed to enhance community well-being, and seed grants for small entrepreneurs who include a well-being focus in their projects. Again, many of the policies were simple and relatively inexpensive, but improved the community’s well-being, as assessed by the annual surveys.
The Center for Creative Healing in the School of Public Health at the University of Louisville is designing and evaluating initiatives that encourage relevant industries—such as health care providers and the makers of athletic equipment—to include and evaluate policies that enhance worker well-being. The center is also active in solutions to address the opioid epidemic and racial division in the city. Importantly, they have the interest and logistical support of key local government officials there.
There are also examples in the arena of mental health. The Maryland Behavioral Health Administration (MBHA) has a wide range of programs to address mental health issues of vulnerable populations in the state, including a program to support the children of opioid patients and teaching them resilience and coping skills, based on age-appropriate messaging. In Wicomico County in southern Maryland, first responders collaborate with mental health care providers when they respond to overdose calls and encourage addicts to get into treatment, following their progress over time, when possible. (COVID-19 has hampered these efforts for obvious reasons). The Center for Healthy Places at Salisbury University, meanwhile, supports these efforts by providing logistical support from rising students in the social work program.
There are also examples of economically oriented solutions for deprived communities. In a 2020 report on community revitalization, Tim Bartik of the Upjohn Institute proposes a federal program to provide block grants (at a cost of $12 billion per year) to communities with a high percentage of out of labor force individuals. The grants would cover economic development and employment and training services, information services, and job retention support, among other things.
These programs likely have more potential than grants to support individuals moving to communities where there are more jobs for two reasons. The first is that, as our work (described above) has shown, these populations tend to not move, either due to health problems, or due to lack of skills and motivation to do so. The second is that the more willing-and-able workers move out of these communities, the lower the chances of revitalizing their labor markets. The provision of new jobs can also have spillover effects and encourage additional labor market participation.19Additional efforts are needed to reach the most deprived—and vulnerable—communities.
Bill Galston and Mark Muro of Brookings, meanwhile, propose strategies to bridge the gap between regional growth poles and left-behind deprived communities. These include narrowing the gap in digital skills and in access to broadband internet, providing capital to businesses in falling-behind places, and identifying linkages to regional growth poles.
Efforts such as these also often require training for new kinds of jobs for the low-skilled as traditional jobs fade. These include training in medium-skill tech support, soft skills, and other less-traditional education, particularly for the youth in these communities. Another policy that could complement these is the creation of a national service program for high school graduates, as Isabel Sawhill and Richard Reeves have proposed. They suggest that those who participate in a year of national service receive a grant for two years of tuition at a public college or university.20 The service program can also serve as a gateway into networks and experiences that youth living in civic deserts lack and be an equalizing force and form of civic education.
What is missing
All these programs can make a positive difference. But they will be much more effective if they are part of a coordinated effort and do not operate in silos. Individuals with very low levels of well-being are unlikely to take up opportunities such as job training programs unless their mental health issues are addressed. Those with opioid use disorder, for example, cannot recover in a vacuum and need access to treatment and follow-up support.
Yet in the U.S. today, insurance for and access to mental health care is extraordinarily weak compared to other wealthy countries. According to SAMHSA, one in five U.S. adults experienced mental illness in 2018 and one in 14 people aged 12 or older had a substance use disorder. Yet in 2017, despite the rising rates of overdoses and suicides, only $1 out of every $100 spent on health care was for addiction treatment, and only $1 out of every $25 was for mental health and substance use disorders combined.
Youth in deprived communities will not participate in job training programs if they have no hope for the future nor awareness of what kinds of opportunities that participation will lead to. First responders will not be very effective at getting those with addiction into treatment if they are not well connected with local treatment providers or aware of what efforts have succeeded and failed elsewhere.
Unless our society’s well-being—including mental health—becomes a national priority, we are unlikely to achieve a complete recovery from the COVID-19 shock. The many local initiatives we have are essentially operating in silos, with little ability to get to a higher scale or to coordinate with other relevant actors elsewhere. And without a federal level commitment to well-being and mental health, the issue is likely to remained sidelined.
One positive sign is that many federal level agencies, such as the Federal Reserve, the Consumer Financial Protection Bureau, the CDC, Health and Human Services, and the Census Bureau, among others, have begun to include well-being questions in their official surveys. Tracking the problem is a first step to mainstreaming the issue.
More important though, is the signal that the creation of a federal entity would send about societal well-being as a national priority, and that in turn would create a momentum of its own. The main objective is not to provide funds on a large scale, but rather to provide logistical support and shared information and to prioritize the issue in the public dialogue. This will not be completely free of cost, but the costs of not addressing the problem will be significantly higher, both in terms of lost productivity and lost lives.
I thank Sarmed Rashid, formerly of the White House Task Force on Opioids, and Amy Liu and Elaine Kamarck of Brookings for very helpful comments.
-
Footnotes
- Those individuals who are no longer looking for work for more than six months drop out of the unemployment rate calculation.
- Graham, C. and Pinto, S. (2019). “Unequal Hopes and Lives in the USA: Optimism, Race, Place, and Premature Mortality,” Journal of Population Economics, Vol. 32:665–733 https://doi.org/10.1007/s00148-018-0687-y.
- Graham, C., and Pinto, S. (2020) “The Geography of Desperation in America: Labor Force Participation, Mobility, Place, and Well-being,” Social Science and Medicine, https://doi.org/10.1016/j.socscimed.2020.113612.
- Herrin, J., Witters, D., Roy, B., Riley, C., Liu, D. and Krumholz, H. M. (2018). “Population well-being and electoral shifts.” PLOS One, 13(3), e0193401.; Pinto, S., Bencsik, P., Chuluun, C., Graham, C. (2020). “Presidential Elections, Divided Politics, and Happiness in the U.S.A.” Economica, doi:10.1111/ecca.12349.
- O’Connor, K., and Graham, C. (2019). “Longer, More Optimistic Lives: Historic Optimism and Life Expectancy in the United States,” Journal of Economic Behavior and Organization, V.168.
- For a review of changing beliefs in the American Dream, see Graham, C. (2017). Happiness for All? Unequal Hopes and Lives in Pursuit of the American Dream (Princeton: Princeton University Press).
- Blanchflower, D. and Oswald, A. (2019). “Unhappiness and Pain in Modern America: A Review Essay and Further Evidence for Carol Graham’s Happiness for All?” Journal of Economic Literature. 57(2), 385–402 (June).
- Funke, M., Shularick, M., and Trebesch, C. (2106). “Going to extremes: Politics after financial crises, 1870–2014,” European Economic Review, Vol. 88 (September), Pp. 227-260.
- The data on fentanyl deaths is from the CDC annual reports; on the mechanics of addiction, see: Satel, S. (2019). “The Truth about Painkiller Addiction,” The Atlantic, August 4.
- Work, Skills, Community: Restoring Opportunity for the Working Class (2019) Joint Report from Opportunity America, The Brookings Institution, American Enterprise Institute: Washington, D.C. See also Sawhill, I. (2018). The Forgotten Americans: An Economic Agenda for a Divided Nation (New Haven: Yale University Press).
- Graham and Pinto, 2020.
- Graham and Pinto, 2020.
- Kerpelman, J. Eryigit, S., Stephens, C. (2008). “African American Adolescents’ Future Education Orientation: Associations with Self-efficacy, Ethnic Identity, and Perceived Parental Support.” Journal of Youth & Adolescence. Sept., Vol. 37 Issue 8, pp. 997-1008.
- See Chapter 4 in Graham (2017) for a summary of trends across races.
- Cherlin, A. (2019). “In the Shadow of Sparrows Point: Racialized Labor in the White and Black Working Classes,” Russell Sage Foundation Working Paper, New York (October).
- Maryland HIDTA (2020). Maryland Operational Opioid Command Center, 2nd Quarter Report, (September).
- Kawashima-Ginsberg, K., Sullivan F. (2017). “Sixty percent of rural Millennials lack access to a political life.” The Conversation, March 27.
- For full disclosure, Graham is on the advisory panel of WWWB.
- These efforts could complement but are distinct from Opportunity Zones, which are aimed at labor markets rather than at more general community renovation.
- Reeves, R. and Sawhill, I. (2020). A New Contract for the Middle Class (Washington, D.C.: The Brookings Institution Press).
The Brookings Institution is committed to quality, independence, and impact.
We are supported by a diverse array of funders. In line with our values and policies, each Brookings publication represents the sole views of its author(s).