Although advancements in medical science have greatly improved overall life expectancy and the ability for many to survive a cancer diagnosis, a recent study predicts that cancer care alone will cost the American health system $157 billion by 2020. It is well known that a major driver of these surmounting costs is the rising cost of chemotherapy and other treatments, in addition to the variation in how these treatments are used across the health care system. However, there are several ways that providers, payers, and patients can work together to establish a more medically and financially effective cancer care model that also reduce costs and inefficiencies in the system.
Figure 1: Estimates of the national expenditures for cancer care in 2010 and estimated increase in cost in 2020
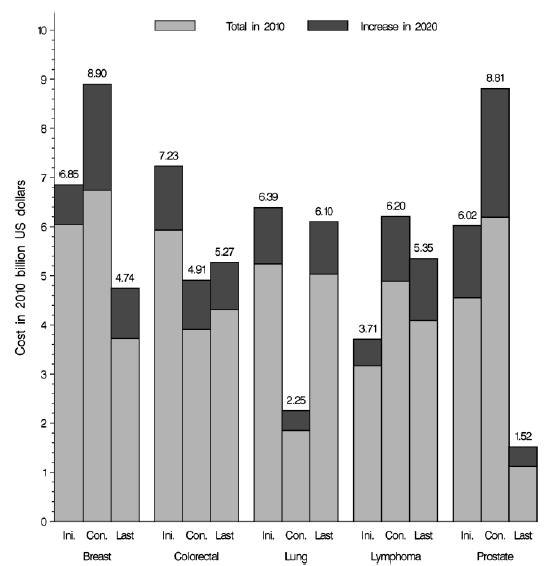
Source:
Journal of the National Cancer Institute
Develop “Clinical Pathways” to Reduce Inappropriate Use
For many cancers, there are multiple drugs that can be equally effective in treating a patient’s condition, but the price of these treatments can differ in cost by tens of thousands of dollars. Currently, oncologists are responsible for purchasing their own chemotherapy drugs, processing and maintaining them in a specialized pharmacy-like set up, and then administering them to their patients. Insurers then reimburse the oncologists for the cost of the drugs plus a margin to defray the price of maintenance and administration. Since oncologists receive a share of their income from the margins on the drugs they prescribe, insurers assert that there is an incentive to prescribe the pricier drugs, even when lower cost options of equal effectiveness exist.
One mechanism for ensuring that the most evidence-based treatment is used in the care of cancer patients is to use a set of “clinical pathways.” These pathways are based on clinical guidelines available to the public, but tailored for a particular set of patients or a type of oncology practice. Many professional societies have contributed to these guidelines and are working on developing more advanced tools to manage a patient’s care. The American Society of Clinical Oncology (ASCO) is developing a system to rate drugs for advanced cancer based on a combination of benefit, side effects and price.
Several health plans and providers are already showing results. A Pennsylvania-based collaboration with the University of Pittsburgh Medical Center and commercial payers achieved savings of more than $1 million in only six months by controlling and reducing the use of Avastin through clinical pathways. A Washington-based health plan also achieved $1 million in cost savings through a partnership with 22 medical oncologists.[i] Most recently, one of the nation’s largest health plans announced a new clinical pathways program that provides oncologists with $350 per patient per month (PMPM) for adhering to specific chemotherapy regimens. The program will be rolled out in July across six states with potential for expansion after its first year.
Develop Appropriate Value-Based Incentives that Improve Care and Reduce Costs
It will also be essential to develop alternative payment models that move away from a volume-based fee-for-service model that only pay oncology practices for traditional face-to-face office visits and parenteral medications. Instead, payers should support the transition to value-based models that reward non-traditional care, such as telephone and e-mail clinician support, patient education, and counseling services with a social worker.
ASCO also released a comprehensive payment reform proposal to transition to an episode-based payment system. The proposal outlines five types of flexible, bundled payments built around (1) taking on new patients; (2) providing treatment during a given month; (3) actively monitoring patients when they are not being actively treated; (4) the progression or recurrence of a patient’s disease that requires significant treatment regimen changes; and (5) a patient’s participation in a clinical trial. Additional recommendations include adding penalties or bonuses of up to 10 percent based on the quality of care provided, and complementing other payment reforms such as primary care medical homes and accountable care organizations (ACOs). A number of potential methods of reforming the oncology payment system have been explored elsewhere, including implementation of the Community Oncology Alliance (COA) Oncology Medical Home.
Replicate value-based models across the private and public sectors. Even with momentum from private insurers, comprehensive change must involve the public sector. When Medicare, the largest health insurer in the country, changes policies, many commercial insurance companies follow suit. Cancer care would be an ideal arena to launch a program like Medicare’s Comprehensive Primary Care Initiative, a multi-payer public sector-private sector collaboration to strengthen primary care.
In many ways, insurers’ decisions to take direct action to minimize variations in care and excessive costs sets the stage for what is to come next in health care reform. Not only does this represent a step toward broad payment reform in oncology, but marks a trend toward exploring new methods of payment in other specialties, and to align those efforts with primary care payment reforms.
To learn more about the Engelberg Center’s efforts to reform payment in the field of oncology, join us on July 9th from 10:30 AM to 12:30 PM EST for MEDTalk: Reinventing Patient-Centered Cancer Care.



Commentary
Op-edChanging the Way We Pay for Cancer Care
June 9, 2014