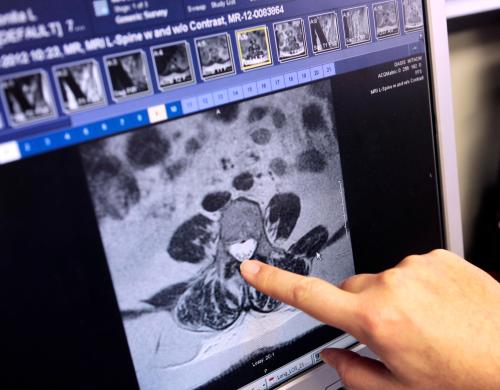
A digitized healthcare system that securely and instantly exchanges medical records between authorized providers, public health agencies, researchers, and patients will radically improve the quality and efficiency of care. An interoperable system across the U.S. is estimated to reduce the overall costs of health care services by $371 billion over 15 years. Given these benefits, the U.S. government has already spent over $35 billion under the meaningful use program to incentivize the adoption of electronic health records (EHR) systems. Despite the fact that almost all providers now use an EHR system, health information is rarely exchanged between them.
To solve this problem, Congress has tasked the Office of the National Coordinator for Health Information Technology (ONC) to “develop or support a trusted exchange framework, including a common agreement among health information networks nationally.” In response, ONC has recently released a draft Trusted Exchange Framework (TEF) in which it first sets six principles for trusted exchange and then briefly describes the minimum requirements to enable the connection between different health information networks.
ONC changes its approach
After reading TEF, I believe that ONC will significantly change its approach towards interoperability. ONC was once saliently involved with rule making and shaping the Health IT market, but is now trying to be truly a “coordinator”, according to Principal Deputy National Coordinator for Health Information Technology Genevieve Morris.
Rather than trying to force the industry to adopt certain approaches, goals, and success metrics, ONC seems to have finally adopted a light-handed regulatory approach. ONC admits that the prior approaches to interoperability have failed. It correctly acknowledges that the health IT ecosystem includes many different stakeholders with their own interests and capabilities, and a mandated single solution to interoperability cannot equally serve all interests. In TEF, ONC has abandoned the idea of combining different health information networks and instead tries to encourage them to “work together to provide that single onramp to Electronic Health Information regardless of what health IT developer they use, health information exchange or network they contract with, or how far across the country the patients’ records are located.”
Facilitating interoperability efforts
Most importantly, ONC has delegated the task of setting and updating detailed terms and conditions for trusted exchanges to a Recognized Coordinating Entity (RCE). As I have written before, the best way to achieve interoperability is through self-regulated, industry driven certification alliances, and I believe achieving this goal by establishing an RCE is a major step in the right direction. However, to ensure that RCE would be successful in paving the way towards interoperability, ONC needs to reconsider how it intends to create and maintain it.
ONC is proposing to select a single RCE through a competitive process that will incorporate minimum interoperability requirements by which qualified Health Information Networks (HIN) may “voluntarily agree to abide”. As ONC has recognized, the success of RCE depends on cooperation of the networks. These entities have very different interests and technical approaches to interoperability. There is no reason to expect that a single industry-based representative be able to incorporate this wide variety of interests and technical approaches and it is very unlikely that all HINs voluntarily agree to its recommendations.
Instead of selecting one RCE to represent the industry, ONC should choose a consortium of industry representatives in which every member of the health IT industry could participate. Health IT entities will not follow the recommendations of the RCE unless they have taken part in designing them and know that such recommendations do not unfairly prioritize the interests of their rivals.
Recognizing business incentives
To enable interoperability, it is important to create business incentives, yet the draft of TEF suggests principles and requirements for which there are no incentives. For example, it asks HINs to “not seek to gain competitive advantage by limiting access to individuals’ Electronic Health Information” and requires them “to not impose any royalty, revenue sharing, or other fee on the use of data once it is accessed by another Qualified HIN.” While I wish that HINs adopted such principles and put societal interests ahead of their own financial benefits, I know that the real world is not so perfect. If some HINs are currently reluctant to share data, what would change in future to lead them to shift their policy and start to willingly exchange their data?
As I have discussed before, unless Congress revises HIPAA and HITECH to allow providers and EHR vendors to charge fees for exchange of medical data, information blocking will continue to be a problem. Legalizing exchange fees would unleash the long-awaited incentives for information exchange in the health care industry and open the floodgates of medical data to allow patients to access, manage, and transmit their medical data as easily as their financial data.
The Brookings Institution is committed to quality, independence, and impact.
We are supported by a diverse array of funders. In line with our values and policies, each Brookings publication represents the sole views of its author(s).







Commentary
To advance health information exchange, we need a health IT consortium
February 27, 2018