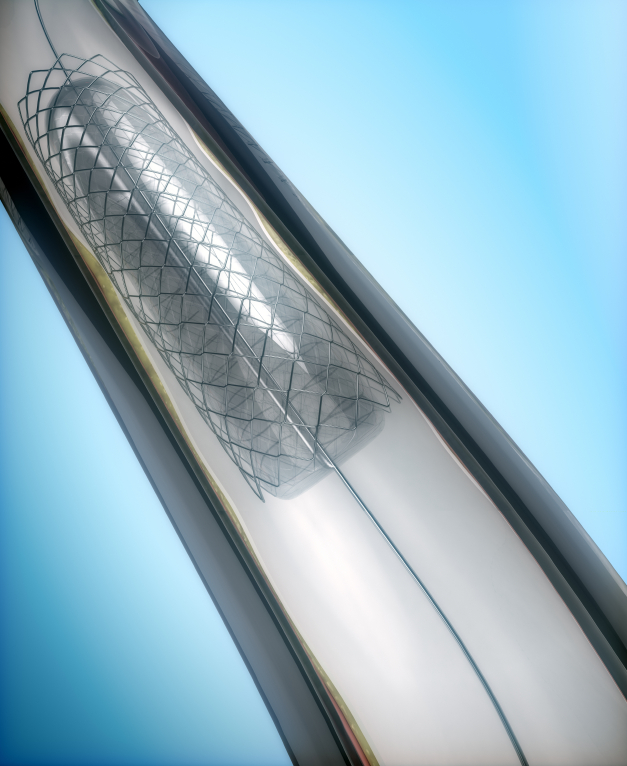
Medical devices play a critical role in health care. Access to reliable and meaningful information about the safety, effectiveness, and quality of devices is essential to inform care and improve patient outcomes. While the Food and Drug Administration (FDA) has a public health mission to monitor the safety and effectiveness of devices, everyone has a vested interest in improving information about medical products. Patients and clinicians need information about devices to inform their clinical decisions. Organizations responsible for paying for care want to ensure that the products they cover lead to optimal patient outcomes. Manufacturers want timely feedback on device performance to support patient safety and drive innovation.
The Center for Devices and Radiologic Health (CDRH) at FDA put forth an action plan to strengthen the nation’s postmarket surveillance system for medical devices in 2012. This plan was developed in response to concerns about the nation’s ability to monitor the safety and effectiveness of medical devices, meet the challenges of supporting medical device innovation, and inform the evolving learning healthcare system. As part of this work, CDRH called for the creation of a multi-stakeholder Planning Board to identify the governance policies, priorities, and business models necessary to develop a sustainable national system for medical device postmarket surveillance. Under a cooperative agreement with CDRH, the Engelberg Center for Health Care Reform at the Brookings Institution convened the Planning Board in 2014. This report represents the Planning Board’s long-term vision for a National Medical Device Postmarket Surveillance System (MDS) and recommended strategies for implementation.
Building a 21st Century Solution
The Planning Board’s recommendations are focused on creating a collaborative system capable of supporting the development, regulation, and use of innovative medical devices. This system should be a component of the emerging national health information infrastructure. It should minimize burden by using data captured as an integral part of care to efficiently generate meaningful and reliable information about medical devices. The system needs to be driven by the need to improve public health and patient care. To accomplish these objectives, the Planning Board proposes the following mission:
The National Medical Device Postmarket Surveillance System (MDS) supports optimal patient care by leveraging the experiences of patients to inform decisions about medical device safety, effectiveness, and quality in order to promote the public health.
To support this mission, MDS should be responsible for coordinating medical devices postmarket evidence activities to ensure that there is a harmonized national approach focused on improving evidence and reducing burden. MDS should also build and facilitate access to network of data partners that utilizes the emerging national health electronic information infrastructure to address medical device specific questions.
The Planning Board does not envision MDS as a stand-alone system. Instead, MDS should build upon and coordinate with other public and private sector existing programs to leverage their expertise and resources. For example, MDS should support Congress’ mandate to include medical devices into the Sentinel Initiative, as well as coordinate with PCORI on their efforts to build a national research network.
MDS’s primary function should be to provide better evidence on the benefits and risks of medical devices to enable active safety surveillance and more effective regulatory decision-making. The system should also seek to collaborate with other groups to support other high-priority evidence needs that could benefit from the same infrastructure, such as product tracking and utilization, clinical quality improvement, and economic analyses of medical device-related care.
The Planning Board recommends that MDS be implemented and managed by a multi-stakeholder public-private partnership with sufficient authority and funding to support its activities. To support broad participation and transparency, the MDS public-private partnership should be built around a set of organizational principles and data governance criteria focused on protecting patient privacy, meeting public health needs, balancing robust analysis and the burden of data collection, and building value for key stakeholders.
Recommended Implementation Approaches and Priorities
Years 1-2: Initiate an incubator project tasked to develop a 5-year implementation plan for MDS through fact finding activities and pilot programs. The Board recommends that the incubator project should be initiated by FDA, adequately staffed and resourced, and guided by a multi-stakeholder group with relevant medical device experience.
Years 3-7: The second phase of work will focus on the MDS implementation plan produced by the incubator project. Once selected, the MDS PPP’s leadership should set and oversee the system’s strategic development priorities, begin to build and sustain broader stakeholder participation, oversee implementation of the organizational plan, and establish system performance measures.
Some of the important challenges the MDS PPP must address during implementation include: (1) supporting a multi-pronged approach to ensure widespread adoption and use of UDIs in electronic health care data; (2) minimizing the burden of data capture and sharing; (3) developing policies to ensure the protection of patients and their privacy; and (4) building the capabilities to provide value to a broad group of stakeholders.
The Planning Board believes that improved medical device surveillance is a public health and national priority and that the most effective way to address this priority is through the broad public-private partnership described in the report.
The Brookings Institution is committed to quality, independence, and impact.
We are supported by a diverse array of funders. In line with our values and policies, each Brookings publication represents the sole views of its author(s).