While American health care does more to improve and extend lives than ever before, overwhelming evidence has shown that outcomes could be substantially better and costs much lower. All over the country, innovative models of health care delivery are being piloted to address these considerations and there are even some pockets of broader adoption. However, the predominant system of payment for health care providers, even in these reformed delivery systems, remains based on fee-for-service (FFS) for specific activities. FFS provides little support for many innovative and personalized services that health care providers are trying to implement to improve health and health care. Many potentially valuable approaches are not reimbursed or are reimbursed poorly, including: team-based approaches to care, systems to coordinate care, virtual and wireless services, and home- and community-based programs that increase convenience for patients and avoid hospitalizations or even traditional office visits. In contrast, traditional FFS payment encourages more volume and intensity of traditional services.
To support innovative, less-costly care, health plans and providers have begun to develop, implement, and evaluate a range of financing reforms. These new models use reimbursement that seeks to reward value rather than volume in order to give providers greater support for delivering care that promotes higher quality and lower costs. The meaning of value is set by the parties in these payment agreements—which typically involve some assessment of quality, safety, and efficiency—with rewards or penalties based on reaching or surpassing predetermined targets. The non-FFS, value-based payment models include episodic or bundled payments, per-member-per-month payments to support patient-centered medical homes (PCMHs) and other delivery transformation models, and shared-savings and shared-risk accountable care organizations (ACOs). These models seek to improve quality and reduce costs through different approaches. Episodic or bundled payments intend to address variation in quality and cost for a particular episode or procedure through retrospective or prospective reimbursement that includes a lump sum for the set (e.g., hip or knee replacement). Population-based payments and ACO programs create incentives to improve overall cost and quality targeted at the management and coordination of care for an attributed population.
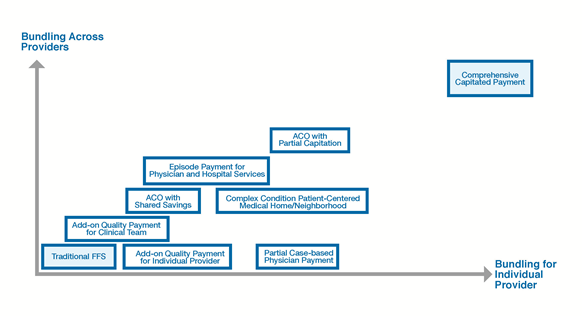
Figure one illustrates the range of value-based payment model options in terms of the extent to which they move away from traditional FFS in the lower left hand corner, and toward more comprehensive, patient-level payments. The figure illustrates how much of the payment shifts from volume and intensity to case- or person-level payment for individual providers on the horizontal axis, and how much it shifts for the other health care providers (e.g., hospitals) on the vertical axis. Such case- and person-level payments are generally tied to the quality and experience of care, and would provide greater rewards than FFS payments for providers that succeed in steps to lower patient-level costs while maintaining or improving quality.
Figure 1: Payment reforms that move away from fee-for-service
In the past few years, health plans and providers have been making notable progress in advancing value-based payments, with plans and providers piloting and expanding a broad range of financing reforms and associated care transformation strategies as they determine which approaches are most likely to be successful in improving care in particular contexts. For example, a recent report by the Blue Cross Blue Shield Association reveals with PCMHs in market or in development in 48 states and the District of Columbia, and ACOs in market or in development in 41 states and the District of Columbia.
In response to growing recognition that the financing of health care must change to support more efficient health care, the adoption of these value-based payment models appears to be accelerating. The Catalyst for Payment Reform estimates that 40% (a 29% increase from 2013) of payments are tied to quality or financial performance or intended to reduce waste. Of these value-based payments, slightly more than half (53%) put providers at risk for costs going up (downside risk) whereas the remaining 47% are financial upside only.
The transition to value-based payments contracts alongside efforts to reform care delivery has been difficult for all involved. It is challenging to develop and implement a model that meets the needs of all stakeholders—providers, payers, purchasers, and members—and that is sustainable in the long- term. This is especially true when the payment reform efforts are undertaken as add-ons to well-established activity-based contract negotiations that focus on price and access for traditionally covered medical services.
The Brookings Institution is committed to quality, independence, and impact.
We are supported by a diverse array of funders. In line with our values and policies, each Brookings publication represents the sole views of its author(s).





