Editor’s note: This blog was written as part of the Center for Health Policy’s Global Accountable Care in Action series that features three long-form case studies focusing on care delivery innovations in Spain, Mexico and India.
View the entire series here
.
Almost 12 percent of Mexican adults have been diagnosed with diabetes and over 60 percent of the population is either overweight or obese, while the prevalence of other chronic diseases is increasing rapidly throughout the country. In response, the Carlos Slim Foundation established the CASALUD program to strengthen chronic disease prevention and treatment throughout Mexico, particularly diabetes, by using health information technology and mobile health (mHealth) platforms.
How does this relate to the U.S.?
More than 9 percent of the U.S. population and over 18 percent of U.S. Hispanics from Mexican descent have diabetes. The U.S. can learn from successful programs in Mexico that promote better patient self-care and clinical management of chronic diseases. Coupled with advances in alternative payment models in the U.S., diabetes programs that offer online patient support and telemedicine for effective disease management could be adopted for high-risk populations.
What lessons can be learned from CASALUD?
The name CASALUD is a play on the words ‘casa’ (house) and ‘salud’ (health) to reflect the patient-focused approach to care. CASALUD provides mHealth tools and technical systems to reengineer how primary care is delivered in clinics to keep patients out of the hospital. The technical tools include mobile screening tools, patient portals, provider education courses, supply chain monitoring, national health statistics, and standardized electronic health records.
At the core of the program is an mHealth platform that directly connects patients to care providers via mobile or web-based program, thereby supporting patients to better manage their own health and become integral members of their care team. A display system called the “operation control board” lists all patient inputs from the mHealth platform helps to improve provider follow-up and encourage more proactive, individualized care. All participating clinics have access to patient files and performance measures, allowing all care team members, including community health workers, provide coordinated care and routine follow-up for better disease management. CASALUD uses technology to improve diabetes screening rates and even clinic infrastructure by ensuring that drugs and commodities are in stock. Figure 1 illustrates the main pillars of the CASALUD model.
Figure 1: The Five Pillars of the CASALUD Model
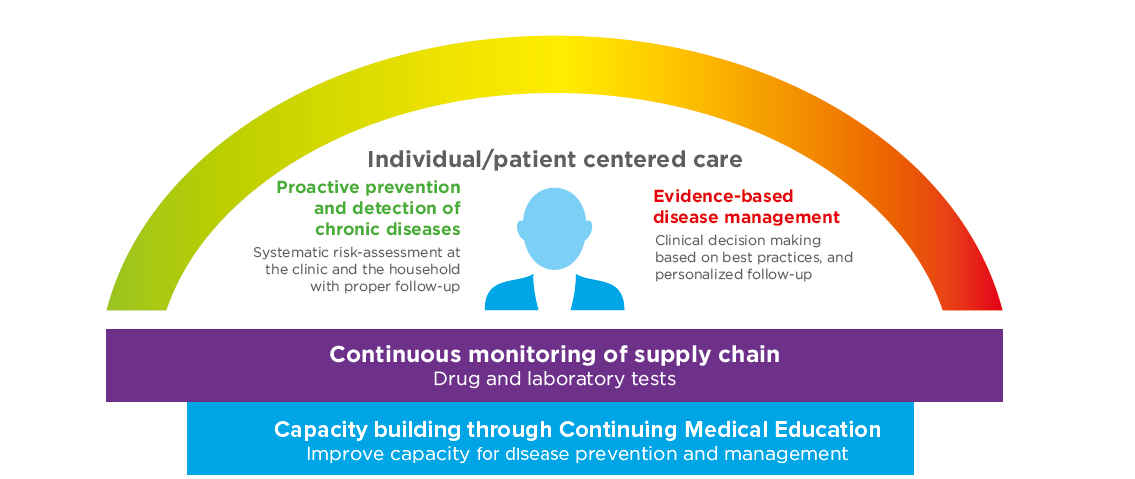
Source: Carlos Slim Foundation
To read more about CASALUD and their notable results, please check out the extended Mexico: Preventing Chronic Disease through Innovative Primary Care Models case study that examines the model according to the Global Accountable Care Framework.
The Brookings Institution is committed to quality, independence, and impact.
We are supported by a diverse array of funders. In line with our values and policies, each Brookings publication represents the sole views of its author(s).




Commentary
What can the U.S. health system learn from Mexico?
April 6, 2015