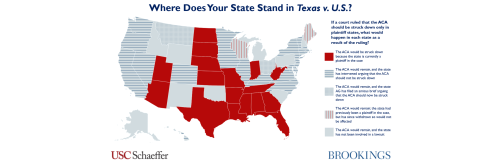
This analysis is part of the USC-Brookings Schaeffer Initiative for Health Policy, which is a partnership between Economic Studies at Brookings and the University of Southern California Schaeffer Center for Health Policy & Economics. The Initiative aims to inform the national health care debate with rigorous, evidence-based analysis leading to practical recommendations using the collaborative strengths of USC and Brookings.
Earlier this year, the Supreme Court agreed to hear Moda Health Plan, Inc. v U.S., a case about the Affordable Care Act’s risk corridors program. Dozens of insurance companies are arguing that they are owed $12 billion in risk corridor payments associated with their participation in the early years of Obamacare. The Court will hear arguments in the case on December 10 and likely make a decision this spring. The Court’s decision will have a one-time effect on the bottom line of many insurers. But how the Court resolves this backward-looking dispute about a now-expired program will not meaningfully change how the Affordable Care Act or health insurance markets operate in the future.
What is the risk corridors program in the Affordable Care Act?
Premiums for insurance products are set in advance, before insurers know what claims spending will be.
That fact can make it hard for insurers to predict what premiums are needed to cover their costs, uncertainty that can be especially large when a new insurance program is launching. The possibility of “guessing wrong” and incurring large losses can make insurers reluctant to participate in insurance markets or overly conservative in setting premiums.
Risk corridors are a standard tool that has been used to avoid these problems by sharing this risk between private insurance companies and the government. If the premium turns out to be too high, so that the insurance company collects far more revenue than is necessary to pay claims, a risk corridor program requires the insurer to pay some of that excess back to the government. Similarly, if the premium is too low and there is less revenue than needed, the government reimburses the insurance company for part of the losses. This creates a stable platform for public-private partnerships, and it can be especially important at the start of a new program when insurers are enrolling populations that they have little experience with.
Risk corridors are part of many existing programs, including Medicare Part D and many state Medicaid managed care contracts. The Affordable Care Act included a temporary risk corridors program, where private insurers and the federal government would share risk for the first three years after the ACA’s insurance reforms took effect – for plans sold in 2014, 2015, and 2016.
While risk corridors have historically been considered technical (and this feature of the law was hardly mentioned in the run-up to passage of the ACA), the law’s risk corridors program became controversial in the years after its enactment. Senator Rubio (R-FL) led an attack on the program as a “bailout” of insurance companies, and a parallel controversy arose over the fact that the ACA had not included an appropriation for funds that might be necessary to make risk corridors payments.
Therefore, as part of budget negotiations in 2014, Republican leaders in Congress insisted that federal appropriations legislation include a provision that prohibited the government from using funds appropriated for the Centers for Medicare and Medicaid Services (CMS, the agency that runs the risk corridors program) to make risk corridors payments. That meant that the government could collect from insurers that set premiums too high and use those funds to pay insurers who set premiums too low, but it would not be able to use other funds to make payments in excess of the amounts collected.
When this provision became law, it was unclear what impact it would have. In the initial years of Medicare Part D, most plans had set premiums too high and the risk corridors program collected more money than it paid out; if the same thing happened in the ACA markets, then the appropriations provision would have no impact. As it turned out, however, insurers had generally priced their plans far too low in 2014, 2015, and 2016 and incurred substantial losses before premium increases returned them to profitability in 2017. Ultimately, in the fall of 2017 when the three-year program concluded, the government owed insurers $12.7 billion, but could pay just $482 million. Not surprisingly, the insurers owed money under the program sued the federal government to collect the remaining funds.
What are the major arguments in the risk corridors litigation?
Dozens of insurers have brought lawsuits to collect the unpaid risk corridors funds. (A court ruling that they are owed the funds would require the government to make payments from a federal account known as the Judgement Fund, notwithstanding the prior appropriations bills.) Insurers are making two broad arguments: First, they argue that the text of the ACA obligated the federal government to pay the full amount due, and that the appropriations rider enacted in 2014 does not affect that obligation. Second, they argue that the federal government also has a contractual duty to pay the full amounts.
The most significant issue in the case is how to interpret the “appropriations rider” that prevented CMS from using its funds to make risk corridors payments. Courts have generally agreed that the text of the ACA initially obligated the government to make risk corridors payments, and that obligation would exist regardless of whether or not Congress subsequently appropriated the funds to make any required payments. But the government argues that the 2014 legislation effectively repealed that requirement – that when Congress said CMS could not use its funds to make good on the obligation, that constituted a repeal of the obligation to make the payments in the first place.
Results in the trial courts were mixed, but the Court of Appeals for the Federal Circuit agreed with the federal government and ruled 2-1 against the insurance companies. The Federal Circuit noted that while so-called “repeals by implication” are generally disfavored, there are a number of Supreme Court and Court of Appeals rulings holding that appropriations bills had repealed the underlying statutory obligation in somewhat similar cases. Those cases generally involve the salaries of government employees, and key precedents date back as far as the 1880s. The appellate court also noted that for the insurers to successful bring a contract claim, they would need to demonstrate that the federal government had an “intent to contract,” and the majority concluded that the statutory scheme precluded the federal government from forming such an intent.
The dissenting judge in the Federal Circuit disagreed with, among other things, her colleagues’ conclusion that the appropriations bill had repealed the ACA’s statutory obligation. She emphasized that the federal government was going back on a representation it made to private parties that they had relied upon when taking on risk that ultimately cost them billions of dollars. In that environment, she argued, the presumption against repeal by implication must be very strong and could not be overcome by the appropriations rider.
The Supreme Court agreed to hear the case and set argument for December 10, 2019.
What impact will a Supreme Court decision in the risk corridors case have?
Many experts were surprised when the Supreme Court agreed to hear the risk corridors case. (In retrospect, perhaps it should not be surprising that the Court took a case involving billions of dollars in payments to private actors for which the lower courts were relying on precedent about government salaries, some of which dates to the 1880s.) Regardless, the Court will decide whether insurers will receive $12 billion.[1] That’s certainly significant for the firms that are owed the funds. But when it comes to health policy, that is just about all the Supreme Court will be deciding.
The risk corridors program expired after 2016. If the Supreme Court rules in 2020 that insurance companies should get paid under the risk corridors program, insurers will receive a large bolus of cash that they “should have” been paid three to five years ago. If the Supreme Court rules against them, they will not. But whether or not insurers are paid does not materially affect how they should price their products for future years or whether they should enter new markets.[2] Those are entirely forward-looking decisions that do not turn on whether insurers are compensated for past-year losses.
That does not mean that the government’s failure to make timely risk corridor payments was harmless. If the risk corridors program had been able to pay the promised funds in those early years, it likely would have had impacts on the ACA markets. Most directly, timely risk corridor payments could have prevented some small insurers who had underpriced from becoming insolvent. Less directly, the absence of risk corridor payments may have been responsible for some of the concerns about market “stability” that dominated ACA conversations in 2016 and 2017. Insurers should have anticipated that it was possible they would underprice in the early years, and when that very pattern emerged, it did not necessarily imply that there were structural problems with the ACA markets. But the unexpected absence of $12 billion that was intended to compensate insurers may have increased the “sting” of those losses or shaken insurers’ confidence, making them more cautious and contributing to insurer exits and premium increases in 2017. And for at least some insurers, depleted reserves may have further contributed to premium increases.
Note, also, that this litigation raises very different issues from another case where insurers have sued the federal government. Specifically, insurers have sued to recover cost-sharing reduction (CSR) payments that the government abruptly stopped making in the fall of 2017 (after making payments from 2014 to 2017). Insurers claim that they are owed the funds the government did not pay for 2017, 2018, and future years. Those cases are still in the lower courts, and, in any case, do not generally involve the sorts of reliance interests that are implicated in the risk corridor litigation: for 2018 and beyond, insurers knew they would not be receiving CSR payments and adjusted premiums accordingly.[3] Therefore, the Supreme Court’s decision in the risk corridor case would not be expected to impact the CSR litigation.
Finally, quite outside the context of the ACA, the risk corridors decision could affect future public-private partnerships — either in health policy or other fields. Specifically, ruling against the insurance companies might affect firms’ and markets’ confidence that future legislation that purports to commit the government to pay a private partner will in fact be binding. That is the key argument made by the Chamber of Commerce, no friend of the ACA, in their amicus brief supporting the insurers in this case. In this respect, the risk corridors case raises an important question of federal policy – but it’s not a question that is of much importance to the future of Affordable Care Act.
[1] Some insurers have sold the right to collect their risk corridors debt to other parties.
[2] It is worth considering how payment of risk corridors funds in 2020 would affect insurer revenue for purposes of the ACA’s medical loss ratio (MLR) requirements. The law requires individual market insurers to spend 80% of the revenue they receive on medical expenses and pay rebates to consumers if they do not. Under current regulations, risk corridors payments are considered revenue in the year in which they are received. If the risk corridors program had operated on the statutory schedule, those payments would have been received in the same time period in which insurers were incurring significant losses on high health care claims, so MLR rebates would generally not have been triggered. Today, however, insurers would receive a bolus of risk corridors payments at a time when they are already profitable, and some may be operating close to the 80% MLR threshold. This could incent some insurers with specific patterns of prior year revenue and costs to offer somewhat lower premiums to avoid having to pay MLR rebates.
[3] In contrast, insurers generally took on risk that was supposed to be “covered” by the risk corridors program before they knew that payments would not (initially) be made. The appropriations rider was enacted in December 2014, after issuers had already contractually committed to their 2015 premiums. And the results from even the first year of the risk corridors program were not known until days before issuers had to make the same commitment for 2016. The three-year results were not known until the fall of 2017, long after the program had expired.





Commentary
The Supreme Court will hear a health care case in December, but its decision on risk corridors won’t affect the ACA
November 4, 2019
Christen Linke Young explains the upcoming Supreme Court case surrounding the ACA’s risk corridor program and why the court’s decision will not meaningfully change how the ACA or health insurance markets operate in the future.