What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Innovation in Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. If you’d like to receive the biweekly Essential Scan by email, you can sign up here.
Florian Heiss, Daniel McFadden, Joachim Winter, and colleagues found that as few as 10 percent of Medicare Part D beneficiaries shopped for and switched benefit plans. Furthermore, most beneficiaries still tended to choose plans that resulted in overspending, though those who switched tended to overspend less on total costs than those who stayed (overspending defined as the difference in all costs including premiums, deductibles, and drug co-pays, relative to the lowest total cost alternative). Using data on Medicare claims and Part D plan selection from 2007 to 2010, the authors explored two channels contributing to the inertia beneficiaries exhibit in choosing plans: inattention to plan choice and perceived costs of switching plans. Events and experiences like hitting the coverage gap or changes in premiums triggered attention to plan choice, increasing the rate of switching and reducing the average overspending rate. But, nearly one third of consumers still chose plans with even higher overspending. Switching and overspending were only moderately improved when the researchers removed all switching costs. These findings highlight the complexity of consumers’ attention to and decision-making skills around benefit plans, complicating policymakers’ task of designing appropriate nudges. Full article here.
Southern US states see highest rates of smoking-attributable cancer deaths
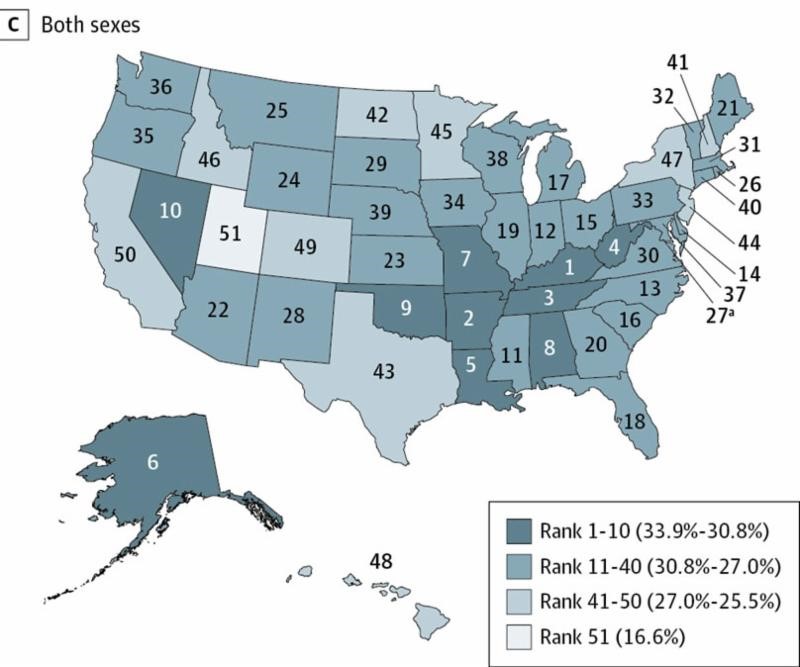
“Local culture clearly plays a role in smoking rates and the resulting deaths from cancer. Cigarette taxes are important as well, but a lot of the variation from state to state reflects culture.”
– Paul Ginsburg, PhD, Director of the Schaeffer Initiative
Joannie Lortet-Tieulent, Ann Goding Sauer, Rebecca L. Siegel and co-authors attributed an estimated 167,133 cancer deaths to smoking in 2014, finding the highest rates of smoking-attributable deaths in southern states. Among men, Arkansas had the highest rate of cancer deaths attributable to smoking at 39.5 percent, though smoking accounted for nearly 40 percent of cancer deaths in five Southern states. Utah had the lowest rates of death: 21.8 percent among men and 11.1 percent among women. The authors point out that few Southern states spend the Centers for Disease Control and Prevention-recommended amount on tobacco control programs, and no states use the World Health Organization guideline of taxing cigarettes at 75 percent of the retail price. Implementing these policies may move the needle on this public health issue. Full investigation here.
Amy N. Finkelstein, Sarah L. Taubman, Heidi L. Allen and co-authors extended their analysis of the 2008 Oregon Medicaid Expansion through a randomized lottery, finding no significant evidence that emergency department (ED) usage decreases over time following Medicaid coverage. Building on prior work that found Medicaid coverage increased usage by 40 percent, the authors analyzed ED use patterns over two years after Medicaid expansion to see if its usage dissipated with time as a result of addressed “pent-up demand.” However, they found no statistically significant evidence of such a decline, noting that Medicaid coverage increased ED usage by 0.17 visits per person in the first six months following coverage, which is 65 percent relative to the mean in the control group of people who were not selected in the lottery, and by 0.15 visits per person in months 18 to 24. These findings complicate earlier assumptions that simply providing Medicaid coverage and access to covered primary care visits might lead to lower utilization of high-cost care like ED visits over time, as Medicaid coverage increased the joint probability of beneficiaries having both an ED visit and an office visit by 13.2 percentage points. It is still possible that some Medicaid beneficiaries are substituting the use of a doctor’s office for an ED for primary care services, but the authors’ findings suggest that any such effect is overwhelmed by increased ED usage resulting from now having Medicaid and presumably greater access to care. Full article here and data here.
2016 silver health plans cheaper on the exchange than off, more likely to be closed-network HMOs
Katherine Hempstead finds that average 2016 silver-level premiums and deductibles were lower on the exchange than off for individuals, yet the share of all plans that had “open” networks was greater off the exchange. Using recently released HIX Compare data that notably includes complete off-exchange offerings, Hempstead found that average silver-level premiums were $279 on- vs. $314 off-exchange, and deductibles had an even greater difference with the on-exchange average at $2,053 vs. $3,273 off-exchange. Overall, 50 percent of off-exchange plans included out-of-network benefits, such as PPOs and POS plans, compared to 36 percent on the exchange. Interestingly, however, the likelihood of such “open” plans decreased as metal tier rose off the exchange, while the inverse occurred on the exchange. These differences between the markets and products raise questions for proponents of a unified individual market as to what impacts these differences may have on the cost and characteristics of plans available to individuals. Full article here.
Lisa Rosenbaum recently authored a three-part series in NEJM probing beneath the surface of current attitudes and policies governing mental health care in the United States. “[In] a country that prizes freedom, the primacy of liberty over need [for mental health care] isn’t surprising,” she writes in Part One. In the vein of the late Oliver Sachs, Rosenbaum brings to light the “rather arbitrary lines in our willingness to treat people who can’t acknowledge their deficits” when distinguishing between issues of mental or physical health, and examines the multifaceted impacts developments like de-institutionalization and the recovery movement have had in caring for individuals with mental health. In Part Two, Rosenbaum highlights the mortality gap experienced by individuals with mental illness, who die an estimated 13 to 30 years earlier than the general population. She assesses the perverse role that assuming a patient’s capacity to deny care can have in avoiding more time-intensive, but perhaps at times warranted, processes of overriding patient choice and underscores the significant impact even small efforts to better understand patients’ reasoning can have in convincing them to follow treatment. Finally, in Part Three, she reflects on how greater efforts to establish trust with patients with serious mental illness, patience and longstanding dedication and flexibility can improve the current state of care for patients. Full articles here, here, and here.
The Essential Scan is produced by the Schaeffer Initiative for Innovation in Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics.






Commentary
The essential scan: Top findings in health policy research
November 3, 2016