Editor’s note: This blog was written as part of the Center for Health Policy’s Global Accountable Care in Action series that features three long-form case studies focusing on care delivery innovations in Spain, Mexico and India.
View the entire series here
.
An estimated 92 percent of all deaths in Spain result from chronic or non-communicable diseases (NCDs). Torrevieja, Spain has the highest concentration of elderly Spanish and foreign retirees in the country– over 25 percent of the population in Torrevieja is above age 65—and has among the highest prevalence of chronic disease. In order to meet and address the needs of the local elderly population, Ribera Salud, a public-private partnership established in Valencia, Spain, developed the Complex Care Plan (Plan de Atención al Paciente Crónico). Ribera Salud has been able to sustain the Complex Care Plan by putting the organization at-risk financially if its patient health costs exceed an established monthly target, or if patients seek care outside of the system.
How does this relate to the U.S.?
Approximately 88 percent of all deaths in the U.S. result from chronic diseases. Approximately 14 percent of the U.S. population is over the age of 65, and this population is anticipated to grow as the Baby Boomer population ages. Physicians, hospitals, and other health care providers need to be better prepared and structured to manage elderly patients inside and outside of hospital settings. The Complex Care Plan serves as an exemplary financial and clinical model to support care transformation for an elderly population.
What lessons can be learned from the Complex Care Plan?
The Complex Care Plan incorporates interdisciplinary primary care teams to coordinate a patient’s care across a range of providers, such as specialists, social workers, nursing facilities, home care aides, mental health providers, caregivers and the patient. Standardized electronic health records and frequent team meetings are used to coordinate the team. The goal of the team structure is to drive patient-centered care to provide more advanced planning, reduce unnecessary hospitalizations, and improve overall care delivery.
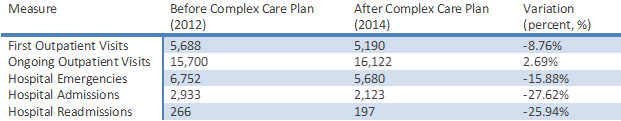
All members of the team, both clinical and non-clinical, receive varying bonuses that are tied to performance measures and based on individual health care plans. Team members can share in savings and can also earn more than a position within the public health care system. Ribera Salud is also at risk if patients seek care outside the system because inevitably the organization will spend more on those services. Since 2012, the Complex Care Plan has resulted in a 27 percent decrease in overall hospital admissions. Figure 1 shows other key results since the beginning of the program.
Figure 1: Key Results Year from 2012-2014
To read more about Ribera Salud and their impressive results, please check out the extended Spain: Reinventing Chronic Care Management for the Elderly case study that examines the model according to the Global Accountable Care Framework.



Commentary
What can the U.S. health system learn from Spain?
April 6, 2015