The COVID-19 pandemic led to a 25 percent increase in the prevalence of mental disorders, particularly anxiety and depression globally according to a 2022 World Health Organization (WHO) report. Among the explanations given for this increase, were the unexpected levels of stress caused by social isolation during the pandemic. Additionally, limits on people’s ability to work and seek support from family, friends, and loved ones were also major stressors that contributed to declines in mental health over the pandemic. These effects were particularly severe for young people, who have a disproportionately higher risk of suicide and self-harming behaviors. All of these results are concerning, especially given the relatively little research available on mental health, and existing evidence that unexpected economic shocks can negatively impact mental health. What policy interventions could improve mental health outcomes? The answer to this question is of pressing policy interest since mental health disorders translate into staggeringly large economic losses, particularly in low-income countries where people are often faced with unexpected shocks to income and health.
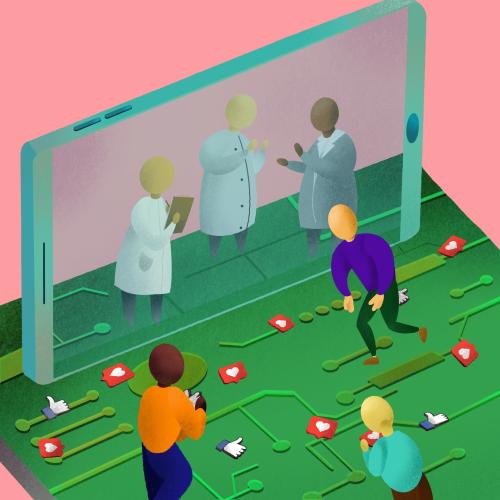
We answer this question using evidence from a communication intervention in Ghana to test whether improved communication, using information and communication technology like mobile phones, can improve mental health. In our study, we partner with a major telecommunications company and implement low-cost communication interventions that provide mobile calling credits to a nationally representative set of low-income adults in Ghana during the COVID-19 pandemic. We find that individuals’ inability to make unexpected calls and need to borrow SOS airtime and seek digital loans decreased significantly relative to a control group. As a result, the programs led to a significant decrease in mental distress (-9.8 percent) and the likelihood of severe mental distress by -2.3 percentage points (a quarter of the mean prevalence). The effects were only through the reduction in mental distress, and there was no impact on consumption spending. Simple cost-benefit analysis shows that providing communication credit to low-income adults is a cost-effective policy for improving mental health. Communication—the ability to stay connected—meaningfully improves mental well-being, and interventions about communication are particularly valuable when implemented as many installments.
Context: The state of mental health and ICT in Africa and globally
While research on mental health is sparse generally, there is very little research on mental health in Africa, a region which faces the joint challenges of high disease burdens and a severely underfunded health sector. According to the 2014 WHO mental health atlas survey, globally, 24 percent of countries reported that they did not have or had not implemented standalone mental health policies. In Africa, the share was almost double that at 46 percent. Based on a recent Lancet study, by World Bank estimates, as of 2017, government spending was just 35 percent of total health spending for countries in Africa, much lower than the world average of 60 percent. Africa’s government spending on health is only 2 percent of GDP—lower than the world share of 3.5 percent. Additionally, out-of-pocket spending as a share of health spending in Africa was among the highest in the world at 37 percent of health spending, compared to 18 percent in the rest of the world. When we add these to the fact that Africa has the world’s youngest population, with 60 percent of the population under the age of 25—and that young people are often identified in the mental health literature as being at high risk for mental health disorders, including suicide and self-harm—then this presents a very worrying picture. At the same time, there are more people with access to information and communication technology (ICT) like mobile phones globally today than at any other point in human history, with the majority of the population in Africa having access to a mobile phone (and over 80 percent of the population in Africa’s most populous country, Nigeria, and the study country Ghana, having access to a cell phone as of 2015). So, can we leverage this near universal access to mobile phones to improve mental health? The study answers this question using evidence from Ghana.
An experimental approach: The effects of ICT on mental health
Administrative data on mobile financial transactions from a major provider in Ghana in 2020 sheds light on the potential value of communication during the pandemic. The data shows that following the onset of the pandemic and the institution of lockdown measures in March 2020, while overall market activity decreased, interestingly and in contrast, demand for mobile airtime-related activities (as measured by the purchase of data and airtime amounts, and thus their demand) sharply increased over the period. In our recent paper, we use a randomized controlled trial (RCT) to estimate the impacts of a short-term “mobile phone calling credit” among a nationally representative set of low-income households in Ghana during the COVID-19 pandemic.
We partnered with a major local telecommunications company to run our experiment by randomly assigning 1,131 individuals to two candidate communication programs: 40GHS ($7.0) lump-sum mobile credit (376 individuals) versus 20GHS ($3.5) monthly installments of mobile credit over two months (371 individuals) versus a control program (384 individuals); and then measuring how these affect individuals’ ability to mitigate unexpected communication constraints during the pandemic, with impacts on well-being, that is, mental health, domestic violence, and consumption expenditures. The different programs about communication provide a means of examining how communication programs might be delivered: One-time large communication transfer versus numerous small installments. Conceptually, programs that facilitate communication during unexpected pandemics could be transformative for people, particularly if bound by internal constraints. Not having to worry about the inability to stay connected could free up the mental and emotional bandwidth needed to thrive through a pandemic and its prevailing uncertainty. The provision of communication credits during these hardships can also directly free up an individual’s resources that would otherwise have been allocated to communication for other consumption expenses. Our interventions are designed to both relax such communication constraints and test their impact on mental health, domestic violence, and consumption expenditures.
We find five set of results, with three main ones detailed below:
- The interventions decreased unexpected communication constraints significantly. That is, our experimental interventions mitigate individuals’ inability to meet unexpected communication needs and stay connected. These effects are larger and more sustained over time for the installment communication credit program compared to the lump-sum credit.
- We find meaningful improvement in psychological well-being, which is measured using the Kessler Psychological Distress Scale (K10). Mental distress decreased (-9.8 percent). Severe mental distress decreased (-2.3pp=-24 percent) relative to a control group. The installment communication credit program had larger and more sustainable effects compared to the lump-sum credit. Relatedly, only the installment program led to a significant decrease in the overall likelihood of individuals threatening their partners by -6.3 percent (but with no impacts on the overall likelihood of individuals hitting their partners—our second measure of domestic violence).
- We find no improvement in direct economic well-being. The overall effect is null on total consumption, which is reassuring since the size and specificity of our intervention were not large enough to meaningfully change consumption. Only the installment communication intervention increased consumption expenditures, but the size is very small economically.
The results suggest that a major policy response to improve mental health, especially during periods of unexpected shocks like epidemics that can negatively impact individual and societal well-being, should be to leverage access to ICT and issue communication credits that make it easier for people to communicate and stay connected to their networks. This is an effective and low cost means of improving mental health, especially in low-income settings where government spending on health and mental health is low.






Commentary
How can information and communication technology be leveraged to improve mental health?
November 2, 2022