Now that the first COVID vaccine, made by Pfizer, is being injected into people’s arms, Americans are anxiously awaiting their turn to get either the two Pfizer vaccine shots or those of at least two other vaccines in the FDA’s approval pipeline, by Moderna and AstraZeneca.
But once those vaccines are widely available, they will not necessarily get us back to normal. Enough of us must be vaccinated to get the country to “true” herd immunity, the point at which the virus begins to gradually die out because it has run out of human “hosts.” Only then will we be able to resume normal family life, schooling, sports events and concerts, and patronize businesses on Main Street (what’s left of it.)
One way to ensure this result: pay people $1000 to take the vaccine, but in two stages: an initial $200 for taking the shot (actually now after the second shot), and the $800 balance when herd immunity is achieved.[1] Assuming 75% of Americans take the vaccine, that means an up-front cost of about $50 billion, and then roughly another $200 billion only if the herd immunity target (discussed below) is achieved. The total price tag is a fraction of the $2 trillion-plus spent on the CARES Act and the added $900 billion relief package congressional negotiators are close to agreeing on at this writing.
The reason for holding out the $800 balance until herd immunity is achieved is to provide strong incentives for everyone to encourage—in real life and on social media— their friends, family, work colleagues, and members of their religious communities to get vaccinated. In social media terms, their taking the vaccine would “go viral,” spread and shared among their network of contacts, increasing the numbers vaccinated.
Key to the proposal, assuming it is needed, is that everyone who takes the vaccine, whenever the payments are offered, gets paid—which ensures that there are no incentives for people to wait for the payment plan to be implemented before getting vaccinated. Of course, paying everyone generates two costs: (1) the cost of overcoming the mistrust of science and our political divisions, and (2) the cost created by free riders, people who don’t need the monetary incentives to be vaccinated. But I believe most Americans and businesses would agree that the benefits of getting the economy and our society back to normal more quickly are well worth the costs.
Over the past four months, variations of the vaccination payment idea have attracted some notable supporters—including well-known economists Steven Levitt, Greg Mankiw, and Nobel prize winner Paul Romer, as well as former Democratic presidential candidates John Delaney and Andrew Yang—as well as some criticism. The idea has not only been of academic interest but has also been discussed in major media outlets, including The New York Times and Vox. Here I clarify the idea, put it in the context of recent advances in potentially effective vaccines, and respond to the critiques because other commentators on the matter may erroneously repeat them.
The vaccination rate required for herd immunity
Professor Michael Osterholm of the University of Minnesota, a member of President-elect Biden’s COVID advisory team, has calculated that given the rate at which COVID is transmitted from person-to-person, the nation, or any region, will achieve herd immunity—ideally from vaccination—once 60-70% have sufficient antibodies. The required vaccination rate for true herd immunity, however, is a bit higher than Osterholm’s conservative 70% figure. That’s because no vaccine is 100% effective.
Data supplied by Pfizer and Moderna indicate 94-95% effectiveness. Both require two doses and Pfizer’s vaccine must be kept at a colder temperature than Moderna’s. The third vaccine, made by AstraZeneca, which is widely expected to receive an EUA early next year, is more stable, requires only one dose, and can be stored in normal refrigerators. However, it is the least effective of the three vaccines to date, at 70%. The Johnson and Johnson vaccine is also very promising, designed to be taken by adults in one dose, easy to store, and expected to be supported by efficacy data released in early January. Depending on the mix of the different types of vaccines distributed throughout the population, herd immunity may not be reached until 75% or more of the U.S. population is vaccinated.[2]
How likely is it that the U.S. will achieve herd immunity?
Although recent polling data indicate that public willingness to take the vaccine has steadily climbed to roughly 60% from pre-election lows in the 40-50% range, it is below where we need to be. However, it is likely that public support will continue to grow because:
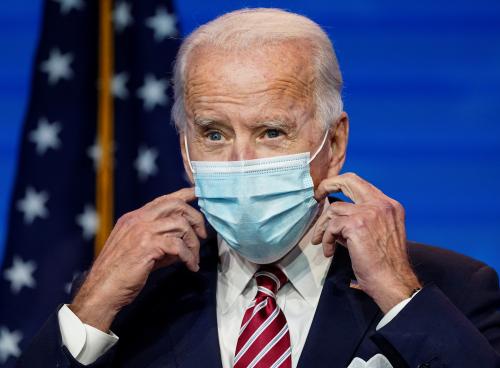
- A major public education program is being ramped up in all the states. Expect to see many celebrities and political leaders, including three former presidents and President-elect Biden taking their COVID shots on television soon.
- As the vaccine becomes available to the general public in the spring, many people who now are on the fence about taking the vaccine should become more comfortable with the idea.
- Similarly, by the spring, more people are likely to be willing to take the vaccine on the advice of their doctors, and because airlines and certain local venues—starting with sports stadiums—likely will require proof of vaccination as a condition of entry (via QR codes or their equivalents available through mobile apps currently under development).
Of course, no one knows whether those influences will be sufficient to get us to where we need to be or whether they may be offset because people do not like the protracted process of taking two shots and because some may experience publicized side effects or severe reactions.
And then, of course, there is the vocal “anti-vaccine” community that will resist taking the shot under any circumstances. The latest polling data suggest that although “anti-vaxxers” account for no more than 5-10% of the U.S. population, some, perhaps many in this camp could use social media to spread misinformation and discourage others from taking the vaccine.[3]
The options for bridging any “vaccination gap”
In short, there is considerable uncertainty about whether, even with an aggressive public education campaign, the vaccination rate will achieve true nationwide herd immunity. If the gap between actual vaccinations and the “required” rate of 75% or higher is small—say a few percentage points—it could make sense for society to live with the virus, counting on continued improvements in therapeutics which have cut the death rate substantially, and a ramping up of production and storage of two of the most effective antibody therapeutics, made by Regeneron and Lilly. Toward this end, the Biden administration should use any available funds to pay for those drugs now, and if additional funds are required, they should be sought upon taking office.
Society is left with only two other options to close any “vaccination gap” to achieve herd immunity. The first, mandating that everyone take the vaccine, would be politically unacceptable and face resistance that would be difficult to address given the extensive resistance by many to wearing a simple mask
That leaves vaccination payments—or a carrot instead of a stick—as the only other option for closing any remaining vaccination gap. I want to stress that the payment plan has been become less essential as support for the vaccines has risen and may continue to rise. However, the payments still merit consideration as a Plan B—or “break the glass” option—if necessary.
Critiques of payment for vaccinations: Rationales for making it Plan B
Framed as a Plan B, the vaccination payment plan would be viewed as a “just in case” economic incentive for individuals to do something in the broader social interest that would enable the United States to reach herd immunity, after everything else has been tried but has still left us uncomfortably short of that goal. Any fiscal stimulus associated with the initial and subsequent payments would be a bonus, not as the main rationale for the idea. The case and eligibility for additional rescue money ideally should be independent of whether the vaccine is taken, not only out of fairness but to avoid charges of compulsion.
Some critics claim that attaching a price to the vaccination could make the subset of holdouts more fearful of accepting the shots by signaling that there may, in fact, be a risk to taking the vaccine. However, by the time the payments are in effect—that is, Plan B—we will have accumulated considerable evidence on the risks of the vaccine, which undoubtedly will be small compared to the risks of becoming seriously ill with the virus. Thus, the payment is likely to offset many individuals’ objections to taking the vaccine and, importantly, induce enough people to take it so we can get over the hump to reach herd immunity.
It has also been argued that the payment plan somehow is unfair to minorities, especially Black Americans, who have shown up in public opinion polling as among the most reluctant to get vaccinated, given the fear that they again will be treated as experimental subjects. The answer to this straightforward: by the time Plan B would be activated, the evidence would be clear that the vaccine is safe for all people to take, including minorities who may need the additional push embodied in a payment to feel completely comfortable about taking the shot(s).
In sum, a vaccination payment is a sound and potentially valuable Plan B. Critics are effectively saying that it is better for the nation to continue to suffer from the fear and the cost of the virus than to pay a modest sum to end this national nightmare. Framed as a cost-benefit assessment, the payment, if needed, is a no-brainer.
[1] In mid-August I proposed in a Brookings piece (https://www.brookings.edu/opinions/want-herd-immunity-pay-people-to-take-the-vaccine/) and expanded the idea in a Milken Review article (https://www.milkenreview.org/articles/paying-our-way-to-herd-immunity).
[2] The vaccination rate at which herd immunity is achieved is conservatively calculated as Osterholm’s estimate of 70 percent divided by the weighted average effectiveness of all the vaccines that are approved and distributed to the public.
[3] Jared S. Hopkins. “One Hurdle on Shot: Convincing Skeptics,” The Wall Street Journal, December 14, 2020. Facebook has announced it will ban anti-vax ads [Link: https://www.cnbc.com/2020/10/13/facebook-bans-anti-vax-ads.html], but not posts on its platform. Instagram and Twitter have not announced bans either.






Commentary
If necessary, the U.S. should pay people to get a COVID-19 vaccine
December 17, 2020