02
Support for public health:
Preparing for the next pandemic
Building a new public health order for Africa—and a new approach to financing it
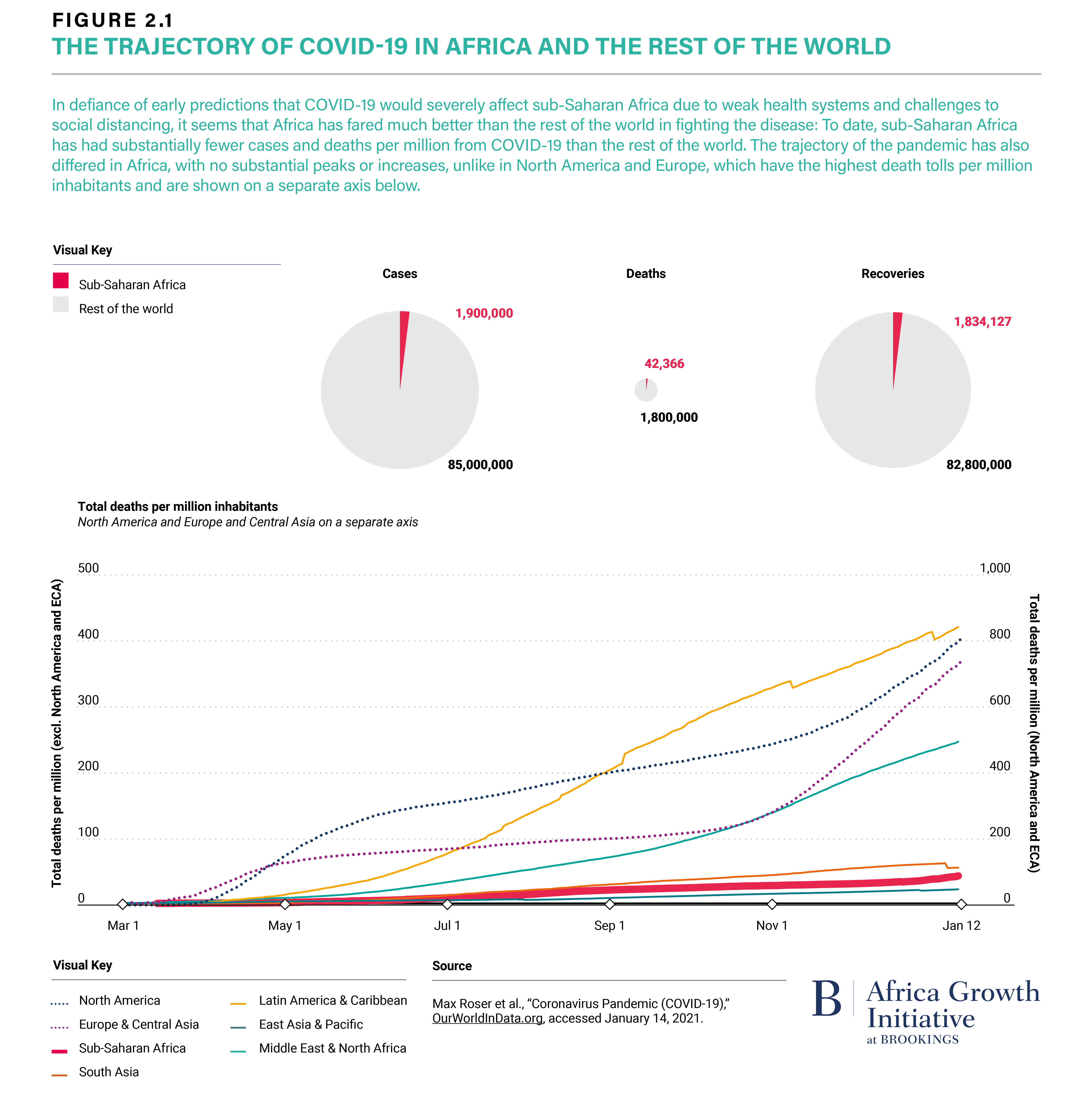
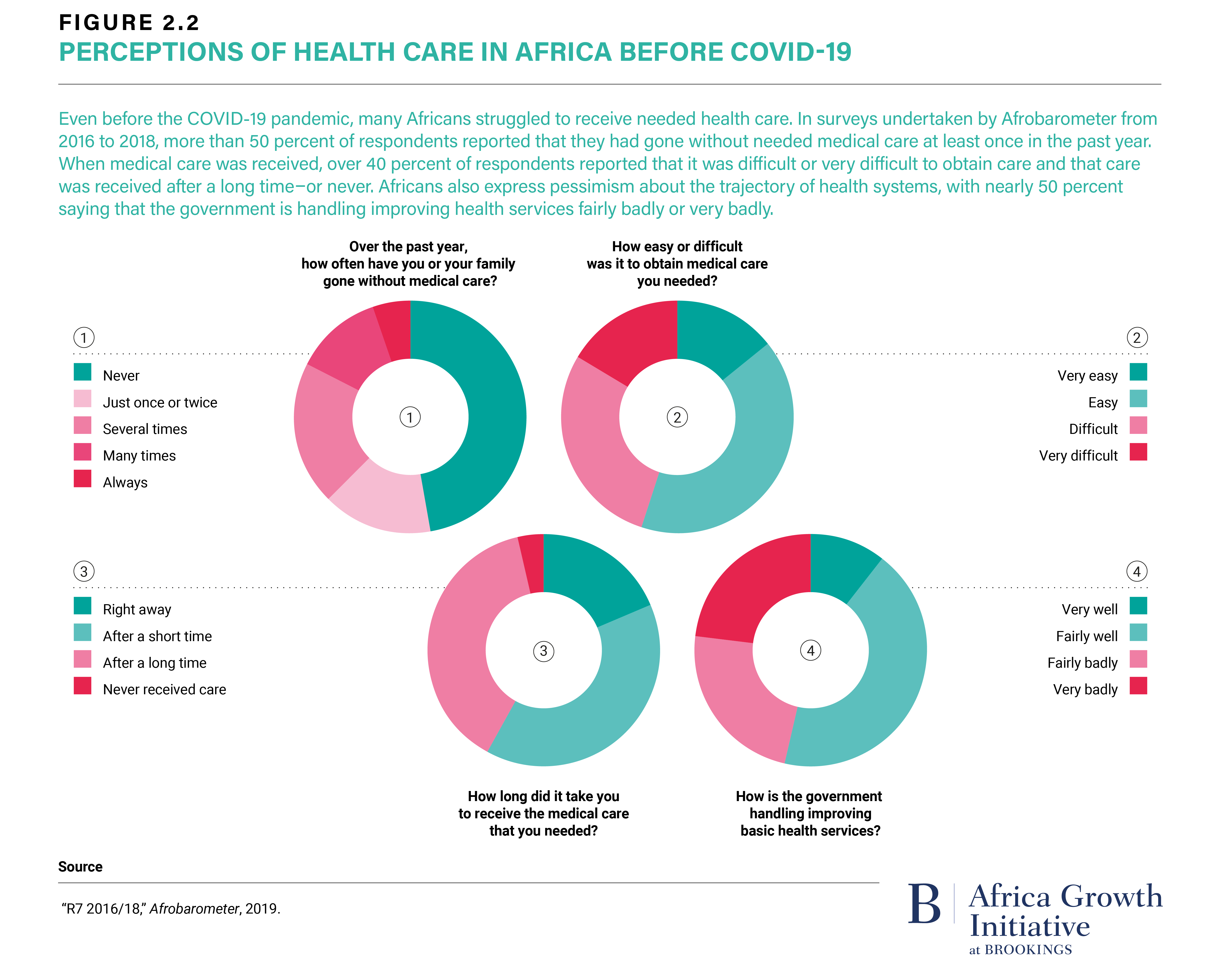
In the early autumn of 2020, Africa received positive press about its response to the SARS-CoV-2 (also known as COVID-19) pandemic. Given the fragility of many of the continent’s health systems, many had initially feared that the impact of SARS-CoV-2 would be devastating. Indeed, Africa has the largest burden of endemic diseases in the world, and SARS-CoV-2 could abolish decades of progress in the fight against these diseases by disrupting health care provision and access to medications. In addition, as the world races for access to critical diagnostics, pharmaceuticals, and vaccines, protectionism rises. With limited local manufacturing capacity, Africa is particularly vulnerable to such dynamics.
Thankfully, as of this fall, Africa had counted just about 1.5 million cases and 40,000 deaths—far, far fewer than other, often richer, regions of the world. Public health experts largely attributed Africa’s success so far to favorable socio-economic, demographic, and environmental factors, but also to rapid and determined political action. Indeed, many African countries were quick to introduce containment measures, such as lockdowns. The continent has also approached the crisis largely as a bloc: Even before the first case was confirmed in sub-Saharan Africa, the health ministers of the member states of the African Union held an emergency meeting to prepare for the pandemic and, fewer than six weeks after the first reported case on the African continent in Egypt on February 14, released the Joint Africa Continental Strategy on COVID-19.
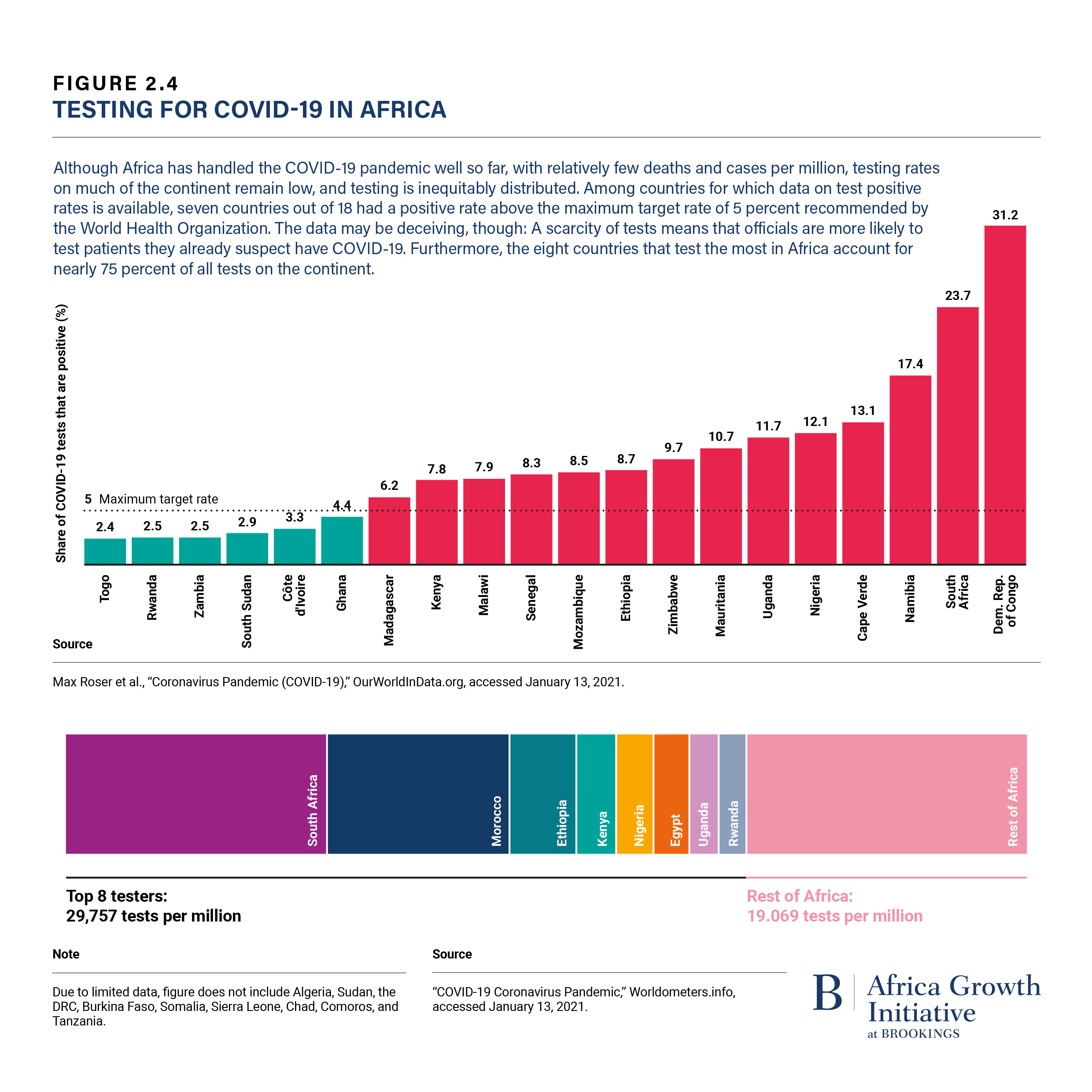
The African approach has been anchored in collaboration and solidarity. Successes include the Partnership to Accelerate COVID-19 Testing (PACT), launched by the African Union Commission (AUC) and the Africa Centres for Disease Control and Prevention (Africa CDC) in April 2020, which enabled Africa, initially shoved aside when global demand for diagnostics rose, to increase the number of countries with testing capacity from two to 43 in three months, procure more than 90 million test kits, and train thousands of lab workers. Similarly, a shared effort among the AU, Africa CDC, UNECA, and the African Export-Import Bank to create the Africa Medical Supplies Platform led to pooled procurement of critical medical supplies, increasing countries’ access to vital personal protective equipment regardless of the size of their market. The most recent example is the Trusted Travel Platform launched by AUC and Africa CDC in October 2020. The platform includes information on the latest travel restrictions and entry requirements and simplified health-related immigration processing for travellers and port officials, which will protect lives and livelihoods and help prepare for the implementation of the African Continental Free Trade Area (AfCFTA).
“The African approach to COVID-19 has been anchored in collaboration and solidarity.”
However, if we only look at SARS-CoV-2-related morbidity and mortality, we miss a large part of the pandemic’s impact and of the underlying vulnerabilities it exposes. To address this multidimensional threat, Africa requires a new public health order, including:
1. A strengthened Africa CDC and national public health institutions (NPHIs). Africa CDC, through its Secretariat and Regional Collaborating Centers, provides national NPHIs with guidance on priorities and programs, integrates efforts, and drives standard-setting and surveillance.
2. Local production of vaccines, therapeutics, and diagnostics that contributes to supply security, drives down procurement costs, and increases the speed of response to a local threat. Such initiatives should be driven by strong private sector partners, with public support for the required capability building and other enablers, but also for the negotiation of contracts that are sufficiently large and long-term for the initiative to attract the required funding. An example of such a public-private partnership is the South African Biovac Institute.
3. Investment in public health workforce and leadership programs. A sufficiently large, well-prepared health workforce is key to any of the activities mentioned above. But the gaps are significant. For example, Africa requires 25,000 frontline epidemiologists and has about 5,000.
4. Action-oriented partnerships—including between the public and private sector, donors and governments, and with public health institutions. Respectful partnerships are those that respect African-originated and defined health priorities and solutions and ensure health programs are aligned with continental priorities such as the Agenda 2063.
This new public health order requires more predictable, long-term funding overall, joint priority setting, and stronger mechanisms to manage the allocation of funds in line with continental aspirations.
Funding in the tens of billions of dollars is required to train the nurses, physicians, and other cadres needed to close the gap in the availability of trained health care professionals predicted for 2030 and create programs for public health policy professionals. Such programs must include support to public health professionals looking to gain additional degrees in health policy, but also opportunities to get exposed to public health policy work in national and international organizations. Beyond training, a better equipped medical system requires local manufacturing capacity, which, in turn, needs significant upfront investment. Laboratories, regulatory capacity, medical materials, and mechanical components for medical tools all require funding.
First and foremost, funding for public health in Africa is the responsibility of the continent’s political leadership. In the 2001 Abuja Declaration, African governments committed at least 15 percent of their annual budgets to health. Since then, only a handful of countries have reached this goal, and overall funding has been inconsistent at best. Policymakers must (re-)prioritize health to consistently reach the commitment of the Abuja Declaration. Second, donor contributions are highly relevant, much appreciated, and will remain key in the foreseeable future. To be effective, these funds need to be in line with national, regional, and continental public health priorities. They should also, where possible, take the form of co-financing to increase sustainability and contribute to the strengthening of public health institutions. Third, the private sector is an important contributor, e.g., through public-private partnerships (PPPs), as a provider of low-cost, for-profit services and expertise for newer areas, such as telehealth.
Investments in a new public health order pay off. Although estimates differ, there is widespread agreement that the return on investment in health is significant. The McKinsey Global Institute’s recent estimate is one of the more conservative and expects a return of 2:1 to 4:1—an estimate that goes beyond money and includes fewer premature deaths, fewer poor health conditions, and extended participation in the labor market—all of which are valid goals in their own right.